Annals of Cytology and Pathology
Multimodal Sampling in Robotic Bronchoscopy: A Retrospective Comparative Analysis of Diagnostic Performance Using ION‑Guided FNA, Surgical Biopsy, and ROSE/Frozen Section in Lung Lesions
Cedars-Sinai, USA
Author and article information
Cite this as
Lee J, et al. Multimodal Sampling in Robotic Bronchoscopy: A Retrospective Comparative Analysis of Diagnostic Performance Using ION‑Guided FNA, Surgical Biopsy, and ROSE/Frozen Section in Lung Lesions. Ann Cytol Pathol. 2025; 10(1): 001-006. Available from: 10.17352/acp.000033
Copyright License
© 2025 Lee J, Fan X, Bose S, This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.Background: Robotic-assisted bronchoscopy using the Ion™ Endoluminal Platform (ION) has emerged as a promising tool for diagnosing peripheral lung lesions. However, the comparative diagnostic performance of fine needle aspiration (FNA), surgical biopsy (SB), and their combination within this context remains underexplored.
Methods: We conducted a retrospective review of 412 cases of ION-guided transbronchial FNA, and SB performed at a single institution between September 2020 and December 2022. Diagnostic yield, sensitivity, specificity, and accuracy were calculated for FNA, SB, and combined FNA+SB approaches. Additionally, we evaluated the diagnostic contribution of rapid on-site evaluation (ROSE) and frozen section (FS) in 198 cases.
Results: The combined FNA+SB approach demonstrated the highest diagnostic yield (76%) and definitive diagnosis rate (67%), outperforming FNA (54%) and SB (70%) alone. Our combined approach diagnosed 81% of malignant lesions, aligning with findings from the TARGET trial. Smaller lesion size was significantly associated with non-diagnostic outcomes (p < 0.0001). ROSE showed limited standalone diagnostic value, with a high non-diagnostic rate and minimal added benefit when combined with FS.
Conclusion: The combination of FNA and SB provides superior diagnostic performance in ION-guided bronchoscopy and should be considered the preferred strategy when feasible. Although ROSE may offer morphological insights in select intraoperative scenarios, its routine use alongside FS may not be justified. A multimodal diagnostic approach enhances accuracy and supports optimal clinical decision-making in lung cancer care.
Key points
Benign lesions were more likely to yield non-diagnostic results, especially when the lesion size was small.
Malignant lesions were more accurately diagnosed using combined FNA and SB.
Multimodal sampling during robotic bronchoscopy enhances diagnostic confidence and reduces non-diagnostic outcomes.
Lung cancer continues to be the second most common cancer in both men and women and remains the leading cause of cancer-related deaths, despite a decline in incidence and mortality rates [1].
Advancements in diagnostic techniques have led to the development of the Ion™ Endoluminal Platform (ION), an FDA-approved, minimally invasive, robotic-assisted bronchoscopy system. This innovative platform provides access to all 18 lung segments and has shown a promising preliminary diagnostic yield of 89% [2].
Within our institution’s experience over 30 months, ION navigation bronchoscopy has provided a sensitivity of 66-68% and a specificity of 99-100% for detecting malignancies [3,4].
This study aims to evaluate and compare the efficacy of Fine Needle Aspiration (FNA) and Surgical Biopsy (SB) in diagnosing lung lesions, to identify the most effective approach for patient care. Additionally, the study explores the utility of Rapid On-Site Evaluation (ROSE) and frozen sections (FS) as diagnostic modalities. By elucidating the optimal use of these techniques, the study seeks to enhance clinical decision-making and improve patient outcomes in lung cancer diagnosis and treatment.
Materials and methods
In this retrospective study, we reviewed 447 transbronchial sampling of lung lesions performed using the ION-navigation bronchoscopy at our institution from September 1, 2020, to December 31, 2022. Patients were included if they had radiologically detected pulmonary nodules or masses suspicious for either malignancy or benign lesions. ION robotic bronchoscopy provides navigated access to peripheral lung lesions, from which clinicians submitted FNA and SB specimens for pathological evaluation. ROSE of FNA smears and/or FS evaluation of biopsy tissue were performed when requested to assist with lesion localization or provide preliminary diagnostic guidance [3.4].
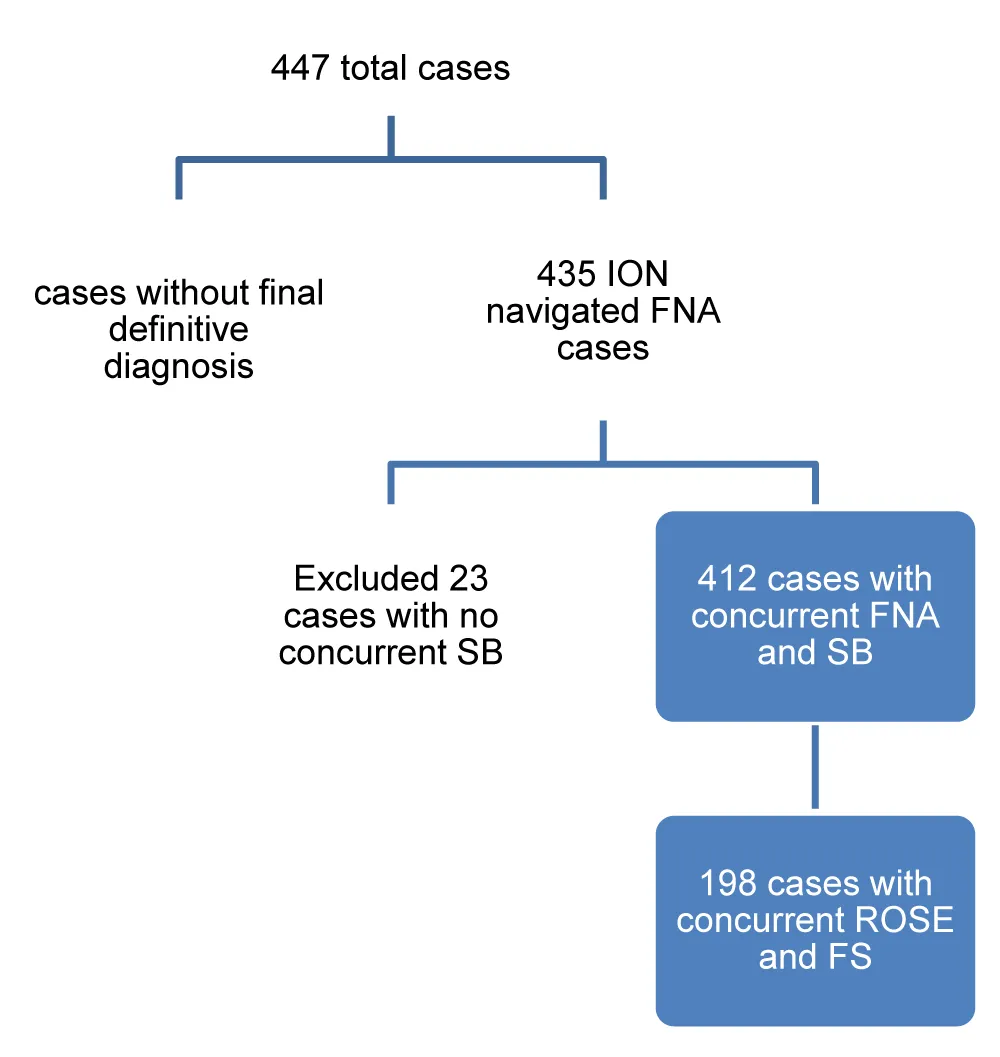
After excluding 12 atypical cases without confirming final diagnoses and 23 cases lacking concurrent biopsies, we analyzed 412 samples from 364 patients. Patients were allocated to diagnostic groups based on the ultimate final diagnosis, which was established through integrated clinical, radiologic, and pathologic findings, including resection specimens when available. Paired FNA and concurrent SB diagnoses were compared, and diagnostic performance metrics, including sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), and overall accuracy, were calculated using Google Colab and the StatsKingdom online statistical calculator, and graphical outputs were generated using Microsoft Excel. Non-diagnostic cases and those in the indeterminate category with atypical diagnoses were analyzed separately. The rate of malignant diagnoses obtained on FNA alone, SB alone, and with combined FNA and SB was determined to evaluate the effectiveness of each sampling technique. Additionally, we assessed a subset of 198 cases with concurrent ROSE and FS to compare their diagnostic efficacy for lung lesions (Figure 1).
Results
We analyzed 412 samples from 354 patients, comprising 190 benign and 222 malignant cases (Figure 2). The diagnoses rendered by FNA and SB were classified according to WHO diagnostic categories: non-diagnostic, benign, atypical, suspicious for malignancy, and malignant [5]. Cases diagnosed as suspicious for malignancy were grouped with the malignant cases since only a small number were present. The combined FNA+SB diagnoses were determined by selecting the higher diagnostic category. The final definitive diagnosis was achieved from a combination of clinical, radiological, and pathological findings from both biopsies and/or resection specimens. The included cases encompassed a broad spectrum of pulmonary pathology, including malignant tumors (adenocarcinoma, squamous cell carcinoma, small cell carcinoma, neuroendocrine carcinomas, pleomorphic/sarcomatoid carcinoma, and metastatic malignancies), low‑grade neoplasms (typical carcinoid tumor, solitary fibrous tumor, and lymphoid neoplasms), and a variety of benign conditions (granulomatous inflammation, infectious and fungal processes, organizing pneumonia, fibrosis, hamartoma, and chronic inflammatory or reactive changes).
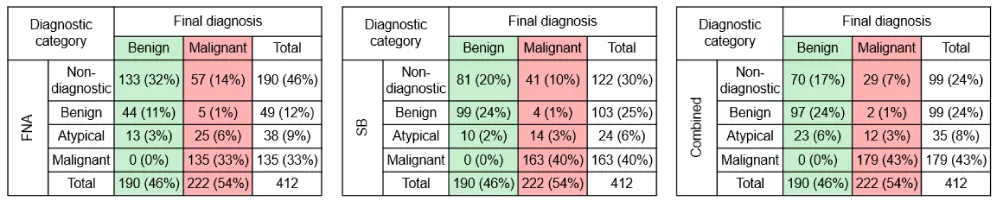
Efficacy among FNA, SB, and combined tests
The study cohort included 190 (46%) benign cases and 222 (54%) malignant cases. Almost half of the studied cases had concurrent ROSE and FS (Figure 2). The diagnoses rendered by FNA, SB, and combined FNA+SB were compared with the final diagnoses (Table 1). FNA alone yielded 46% non-diagnostic, 12% benign, 9% atypical, and 33% malignant results. SB alone produced 30% non-diagnostic, 25% benign, 6% atypical, and 40% malignant results. The combined approach resulted in 24% non-diagnostic, 24% benign, 8% atypical, and 43% malignant diagnoses. The concordance rate between FNA and SB was 81% (161 out of 199) among cases where both were diagnostic, indicating strong agreement.
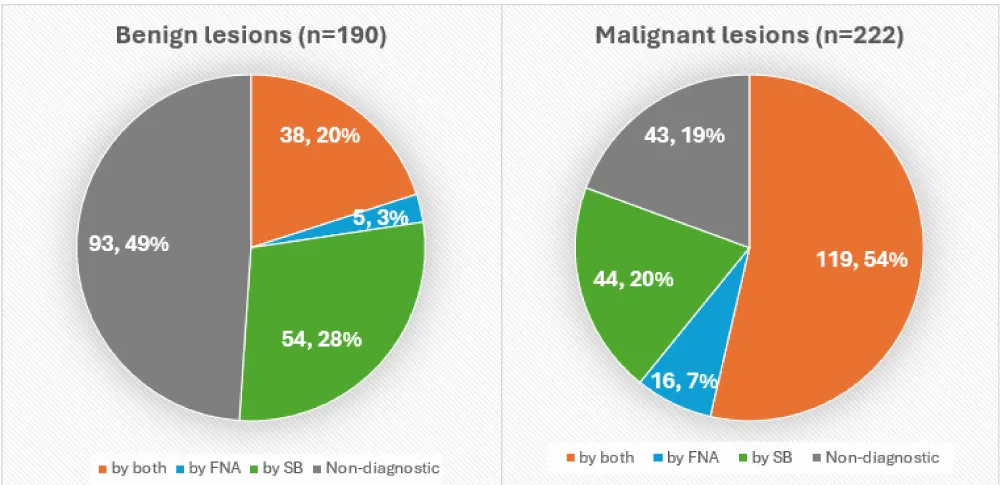
The sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), and overall accuracy were comparable across FNA, SB, and the combined approach. Notably, 23 cases had diagnostic material only on FNA and 91 only on SB, underscoring their complementary roles. Specifically, 16 malignant cases (7%) and 5 benign cases (3%) were identified only on FNA, while 44 malignant cases (20%) and 54 benign cases (28%) were identified on SB only.
The overall diagnostic yield was highest with the combined FNA+SB approach at 76%, followed by SB alone at 70%, and FNA alone at 54%. Moreover, the combined method achieved the highest rate of definitive diagnoses (67%), highlighting its effectiveness in reducing non-diagnostic outcomes (Table 2).
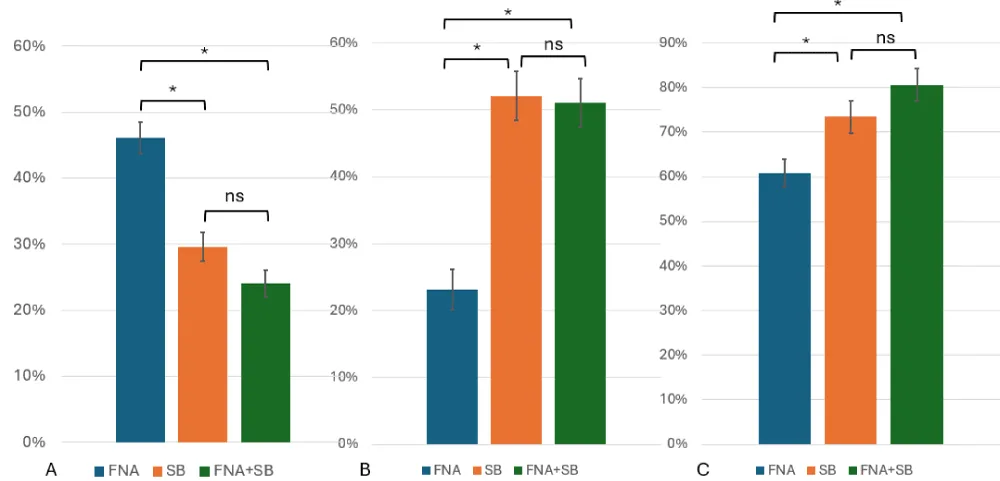
FNA was comparable to SB in diagnosing malignant lesions, whereas SB demonstrated greater performance in identifying benign cases. The combined approach yielded the highest overall diagnostic performance, particularly in detecting malignancies (Figure 3).
Non-diagnostic rate
The non-diagnostic rate varied significantly among the three testing modalities, with FNA showing the highest rate at 46%, compared to 30% for SB and 24% for the combined approach (Table 2). This difference highlights the superior reliability of SB in obtaining adequate diagnostic material, particularly in benign lesions.
To better understand the factors contributing to non-diagnostic outcomes, we examined variables such as lesion laterality, lobar location, operating surgeons, nature and size of the lesion, and total number of smears examined. Although right-sided lesions were more prevalent (270 vs. 142) in the studied cases, neither laterality nor lobar location influenced diagnostic yield. The three primary surgeons had non-diagnostic rates ranging from 20% to 28%, which were not statistically significant.
The nature of the lesion had a notable impact on diagnostic success. Malignant lesions (n=179, yield of 81%) had a significantly higher diagnostic yield compared to benign lesions (n=97, yield of 51%) (Figure 4). SB was particularly effective in obtaining diagnostic material from benign lesions, reinforcing its value in such cases.
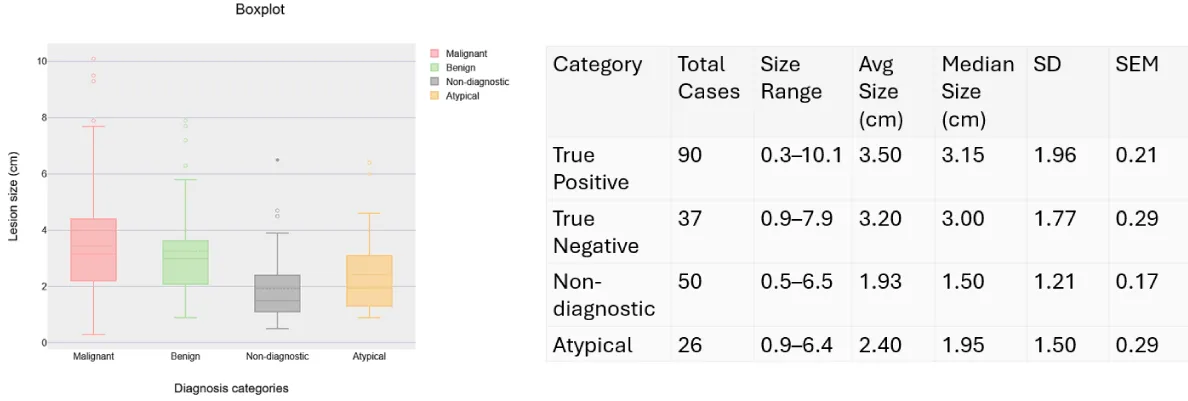
Among the 206 cases with available radiological measurements, lesions that received definitive diagnoses had an average size of 3.38 cm, significantly larger than the 2.09 cm average for non-diagnostic cases; a difference of 1.29 cm (95% CI: 0.80–1.78, p < 0.0001). When stratified by diagnostic category, malignant lesions averaged 3.50 cm, benign lesions 3.20 cm, atypical lesions 2.40 cm, and non-diagnostic lesions 1.93 cm (Figure 5).
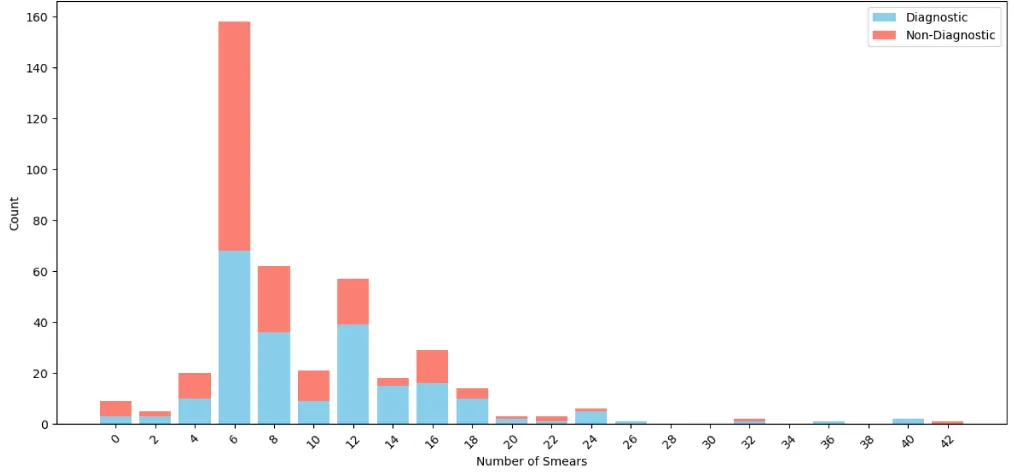
We also analyzed whether the number of smears affects the diagnostic yield. The majority of cases had 6 smears, with 57% of those being non-diagnostic. Cases with 12 smears, 14 smears, and 24 smears had the lowest non-diagnostic rate, but on further analysis, it was observed that these cases were associated with malignant diagnoses (Figure 6).
Among all the variables examined, the nature and size of the lesion were critical factors influencing diagnostic outcomes, whereas the operating surgeon, anatomical access, and smear count did not appear to limit diagnostic effectiveness in this cohort.
Indeterminate category
Indeterminate (atypical) diagnoses were made when lesional cells lacked sufficient quality or quantity. The consideration of atypical diagnoses may vary from reactive changes from various insults to malignancy. FNA had a slightly higher atypical rate (9%) than SB (6%) or the combined method (8%), though not statistically significant. Among atypical cases diagnosed by FNA alone, 66% were later confirmed to be malignant, compared to58% of only atypical cases. In combined cases, 66% were benign and 34% malignant, suggesting that the combined approach may reduce diagnostic uncertainty in atypical cases (Table 1).
Rate of malignancy
Figure 7 illustrates the malignancy rates across different diagnostic categories. The non-diagnostic category showed a malignancy rate ranging from 29% to 34%, indicating a substantial proportion of missed malignancies. The benign category had a relatively low malignancy rate, ranging from 2% to 10%, suggesting good specificity. The atypical category exhibited a wide malignancy rate of 34% to 66%, reflecting greater diagnostic uncertainty. As expected, the malignant category demonstrated a 100% malignancy rate in our study, confirming the accuracy of definitive malignant diagnoses.
Contribution of ROSE in diagnosis
In our study, the diagnostic concordance between ROSE and FS was 62%, with agreement in 40 out of 65 cases. ROSE yielded diagnostic results in 7 cases where FS was non-diagnostic, whereas FS provided diagnoses in 74 cases where ROSE was non-diagnostic (Table 3).
ROSE exhibited a significantly higher non-diagnostic rate and showed limited utility in identifying benign lesions. In contrast, FS and the combined ROSE+FS approach exhibited comparable diagnostic performance, suggesting that ROSE added minimal incremental value when used alongside FS. Notably, atypical findings identified by ROSE were associated with a high malignancy rate (96%). However, ROSE also had a higher false-negative rate compared to FS and the combined method (Figure 8).
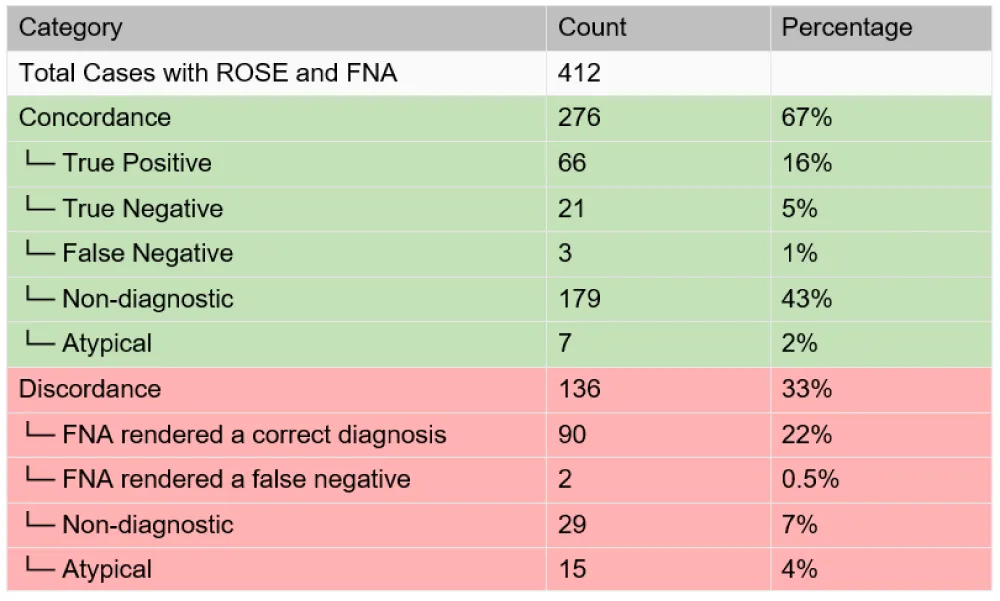
Among the 412 cases with both ROSE and FNA performed, there was a 67% concordance rate between ROSE and FNA results. Of these, a substantial portion (43%) was non-diagnostic. In discordant cases, FNA provided the correct diagnosis in 90 cases (22%), while 44 cases (11%) remained inconclusive (Figure 9).
Discussion
This study provides a comprehensive evaluation of the diagnostic performance of FNA, SB, and the combined approach in the context of ION-guided robotic-assisted bronchoscopy for lung lesions. Our findings underscore the superior diagnostic yield and accuracy of the combined FNA+SB approach, particularly in detecting malignancies, aligning with outcomes reported in the 2024 TARGET trial [6].
The combined modality achieved a diagnostic yield of 76% and an 81% malignancy detection rate, outperforming FNA alone (54%) and SB alone (70%). This suggests that leveraging both cytological and histological sampling enhances diagnostic confidence and reduces non-diagnostic outcomes. Notably, SB demonstrated greater efficacy in identifying benign lesions, likely due to its ability to preserve tissue architecture, while FNA remained valuable in settings where SB was not feasible. Importantly, the combined approach not only improved sensitivity and accuracy but also reduced the rate of non-diagnostic and atypical results. This suggests that a multimodal strategy is essential for optimizing diagnostic confidence, particularly in complex or ambiguous cases.
Lesion size emerged as a critical determinant of diagnostic success. Smaller lesions (<2 cm) were significantly associated with non-diagnostic outcomes, consistent with prior literature [6,7]. Despite this, the ION platform showed promise in diagnosing lesions as small as 3 mm, highlighting the technical precision and diagnostic potential of robotic-assisted bronchoscopy in very small lesions. The study also highlighted the limitations of smear count as a predictor of diagnostic success. The non-diagnostic rate fluctuated significantly across smear counts without statistical significance. This indicates that smear quantity alone does not guarantee diagnostic adequacy.
Among all the variables examined, the nature and size of the lesion were critical factors influencing diagnostic outcomes, whereas the operating surgeon, anatomical access, and smear count did not appear to limit diagnostic effectiveness in this cohort. Our findings are broadly consistent with other previous studies’ observation of reporting diagnostic yields ranging from 70% to 90% [8,9].
The role of ROSE of FNA materials was assessed within this cohort. Although ROSE occasionally offered morphological insights, particularly in cases where FS quality was suboptimal, its overall diagnostic utility was limited. ROSE demonstrated a high rate of non-diagnostic outcomes and provided minimal additional value when used in conjunction with FS. Nonetheless, ROSE may still serve a supportive role in select intraoperative scenarios. In our clinical workflow, smears were received for ROSE while fresh biopsy tissue was processed for FS. Although FS has limitations such as limited tissue availability and freezing artifacts, ROSE specimens could occasionally provide superior morphological detail. This is particularly valuable when FS quality was compromised, allowing ROSE to offer complementary insights that enhance overall diagnostic accuracy.
This study is limited by its retrospective, single-institution design, which may affect the generalizability of the findings. The diagnostic performance of FNA, SB, and ROSE may vary across institutions due to differences in operator expertise, specimen handling, and pathology interpretation. Additionally, the relatively high rate of non-diagnostic FNA cases may be attributed to differences in sampling techniques and lesion accessibility, which were not fully addressed in this study.
Future research should focus on prospective, multicenter studies to validate these findings across diverse clinical settings. Stratifying cases by lesion characteristics, such as size, location, and radiologic features, may help refine selection criteria for FNA, SB, or both. Integration of molecular diagnostics for FNA samples, artificial intelligence-assisted cytology, and real-time imaging enhancements could further improve diagnostic yield and reduce non-diagnostic outcomes. Additionally, cost-effectiveness analyses comparing combined versus single-modality approaches would provide valuable insights for optimizing resource allocation in clinical practice.
Conclusion
This study highlights the complementary roles of FNA and SB in the diagnosis of lung lesions using ION navigated bronchoscopy. While SB alone demonstrated superior performance in diagnosing benign lesions and reducing non-diagnostic outcomes, FNA alone remained a valuable, minimally invasive tool—particularly in settings where SB is not feasible.
The combined use of FNA and SB yielded the highest diagnostic accuracy, sensitivity, and specificity, supporting its adoption as the preferred strategy when feasible. Although ROSE showed limited standalone diagnostic value and a high non-diagnostic rate, it may still offer morphological insights in select intraoperative scenarios, particularly when FS quality is suboptimal.
Overall, a multimodal diagnostic strategy that leverages the strengths of each modality can enhance diagnostic confidence and improve patient outcomes in lung cancer care. Based on our findings, we recommend the combined use of FNA and SB whenever possible, as it offers the most comprehensive and reliable diagnostic performance.
- American Cancer Society. Cancer Facts & Figures 2025. Atlanta (GA): American Cancer Society; 2025. Available from: https://www.cancer.org/research/cancer-facts-statistics/all-cancer-facts-figures/2025-cancer-facts-figures.html
- Intuitive Surgical. Ion™ Endoluminal Platform: Research Outcomes [Internet]. Sunnyvale (CA): Intuitive Surgical; [cited 2025 Jun 15]. Available from: https://www.intuitive.com/en-us/products-and-services/ion/research-outcomes
- Boac BM, Kanathanavanich M, Li X, Imai T, Fan X, Walts AE, et al. Marchevsky AM, Bose S. Accuracy and efficacy of Ion robotic-assisted bronchoscopic fine needle aspiration of lung lesions. J Am Soc Cytopathol. 2024;13(6):420–430. Available from: https://doi.org/10.1016/j.jasc.2024.08.129
- Kanathanavanich M, Li X, Boac B, Bose S, Walts AE, Imai T, et al. Chaux G, Brownlee A, Marchevsky AM. Robotic-assisted bronchoscopy for the diagnosis of lung lesions: experience with the use of frozen sections as an aid to confirm the localization of lesions during the procedure. Arch Pathol Lab Med. 2025;149(3):288–292. Available from: https://doi.org/10.5858/arpa.2023-0458-ra
- International Academy of Cytology; International Agency for Research on Cancer; World Health Organization Joint Editorial Board. WHO Reporting System for Lung Cytopathology [Internet]. Lyon (France): International Agency for Research on Cancer; 2022 [cited 2025 Apr 26]. Available from: https://tumourclassification.iarc.who.int/login?redirecturl=%2Fchapters%2F48
- Murgu SD, Sterman DH, Chen A, Yasufuku K, Pederson D, Rafeq S, et al. A prospective, multicenter evaluation of safety and diagnostic outcomes with robotic-assisted bronchoscopy: results from the TARGET trial. Chest. 2024;166(4):A5268–A5270. Available from: https://doi.org/10.1016/j.chest.2025.04.022
- Li XM, Bai JM, Zhou XM, Wang T, Zhang Y, Hu Y. Diagnostic performance and safety for robotic-assisted bronchoscopy in pulmonary nodules: a systematic review and meta-analysis. Int J Surg. 2025;111(6):4020–4032. Available from: https://doi.org/10.1097/JS9.0000000000002423
- Zhang C, Xie F, Li R, Cui N, Herth FJF, Sun J. Robotic-assisted bronchoscopy for the diagnosis of peripheral pulmonary lesions: a systematic review and meta-analysis. Thorac Cancer. 2024;15(7):505–512. Available from: https://doi.org/10.1111/1759-7714.15229
- Chang AT, Chan JW, Siu IC, Liu W, Lau RW, Ng CS. Robotic-assisted bronchoscopy—advancing lung cancer management. Front Surg. 2025;12:1566902. Available from: https://doi.org/10.3389/fsurg.2025.1566902
Article Alerts
Subscribe to our articles alerts and stay tuned.
 This work is licensed under a Creative Commons Attribution 4.0 International License.
This work is licensed under a Creative Commons Attribution 4.0 International License.




 Save to Mendeley
Save to Mendeley
