Annals of Cytology and Pathology
Diagnostic significance of combined immunohistochemical panel of p63, High Molecular Weight Cytokeratin (34betaE12) and α‑Methyl Acyl Co A Racemase (AMACR) in resolving suspicious foci in prostatic lesions
Nida Malik1, Veena Maheshwari2, Mohsin Aijaz3* and Nishat Afroz2
2Professor, Department of Pathology, Jawaharlal Nehru Medical College, Aligarh Muslim University, Aligarh (202002), U.P, India
3Assistant Professor, Department of Pathology, Faculty of Medicine, Aligarh Muslim University, Aligarh (202002), U.P, India
Cite this as
Malik N, Maheshwari V, Aijaz M, Afroz N (2022) Diagnostic significance of combined immunohistochemical panel of p63, High Molecular Weight Cytokeratin (34betaE12) and α‑Methyl Acyl Co A Racemase (AMACR) in resolving suspicious foci in prostatic lesions. Ann Cytol Pathol 7(1): 029-034. DOI: 10.17352/acp.000026Copyright License
© 2022 Malik N, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.Background: The assessment of small foci of atypical glands in prostatic needle biopsy specimens is a key diagnostic challenge in routine histopathology for pathologists. Due to the presence of mimickers of prostate carcinoma, at times making a definitive diagnosis becomes difficult. The use of immunomarkers like α‑Methyl Acyl Co A Racemase (AMACR), p63 and High Molecular Weight Cytokeratin (HMWCK/34betaE12) has made it easier for us to reach the diagnosis in such cases.
Material and methods: All the cases which were received in the Department of Pathology, JNMCH, AMU from January 2015 to December 2018 were categorized into four histomorphologic groups on the basis of histopathology, and immunohistochemistry was applied on all the cases which were rendered ‘suspicious’ on histomorphology.
Result: One hundred twenty-one prostatic specimens were received. Out of which, 13 biopsies were found to be inadequate for analysis and hence were not included in the study. Out of the rest 108 cases, (1) 52 were benign, (2) 19 were premalignant, (3) 25 were carcinoma and (4) 12 were signed as ‘suspicious’ on histopathology. These 12 suspicious cases were true cut needle biopsies which were considered appropriate for applying immunomarkers along with control cases. Out of 12 suspicious cases, 8 cases (66.7%) were negative and 3 cases (25%) were weakly positive for p63, 1 case showed moderate immunostaining. HMWCK was completely negative in 7 cases (58.33%), 3 cases (25%) showed weak positivity, 1 case showed moderate and 1 case showed strong positivity. While 5 cases (41.67%) were negative and 7 cases (58.33%) were positive for AMACR mostly showing moderate to strong positivity
Conclusion: The application of immunomarkers helped us to reach a definite diagnosis in 10 out of 12 cases, which were otherwise difficult to classify. Judicious use of immunomarkers can help in differentiating mimickers of prostate carcinoma from true cancer cases and assist in reaching a definitive diagnosis.
Abbreviations
AMACR: α‑Methyl Acyl Co A Racemase; ASAP: Atypical Small Acinar Proliferation; BPH: Benign Prostatic Hyperplasia; DAB: Diaminobenzidine; H&E: Hematoxylin and Eosin; HGPIN: High-Grade Prostatic Intraepithelial Neoplasia; HMWCK: High Molecular Weight Cytokeratin; IHC: Immunohistochemistry; LGPIN: Low-Grade Prostatic Intraepithelial Neoplasia; TURP: Transurethral Resection of Prostate
Introduction
There has been a gradual increase in the incidence of prostate cancer since the 1960s in countries with both high as well as comparatively lower incidence e.g. India [1]. The worldwide Prostate Carcinoma burden is expected to grow to 1.7 million new cases and 0.499 million new deaths by 2030 simply due to the growth and aging of the global population [2]. The increase in prostate needle biopsy and hence procurement of minimal tissue as well as progress in our knowledge of mimickers of prostatic carcinoma including prostatic intraepithelial neoplasia, sclerosing adenosis, atypical adenomatous hyperplasia, cribriform hyperplasia, basal cell hyperplasia, etc. have made it necessary to have a keen approach to diagnose these lesions correctly. Accurate diagnosis of these specimens is of utmost importance because if diagnosed early for malignancy, the patient is benefitted as a result of a lesser invasive procedure, compared to more radical procedures in advanced stages that are associated with significant mortality and morbidity.
Although most of the cases are easily categorized as benign or malignant on the basis of histopathology there are few cases, considered as ‘suspicious for malignancy’ which are difficult to classify and pose a diagnostic dilemma to the histopathologists. The aid of immunomarkers like basal epithelial cell markers and prostate carcinoma-specific markers is necessary in such suspicious cases. The aim of our study was to assess the performance of a triple-antibody immunoassay (p63, HMWCK, and AMACR) in evaluating problematic foci in the routine surgical pathology practice involving prostatic specimens.
Material and method
This study was carried out on the patients having either benign or malignant lesions of the prostate, from 2015 to 2018, with a one-year retrospective analysis and two and a half years of a prospective analysis. A total of 121 cases were collected and studied. These included 28 TURP (Transurethral resection of the prostate) specimens, 78 needle biopsies and 15 prostatectomy specimens. Out of which, 13 cases were excluded due to inadequate material and biopsy being non‑representative. Relevant clinical information (history, examination, and investigatory findings) of the cases were collected from the Data and Recordkeeping section of the histopathology lab. The hematoxylin-eosin (H and E) stained slides of all the cases were reviewed by two experienced pathologists and divided into four categories/groups. Benign (52 cases), premalignant (19 cases), malignant (25 cases), and suspicious (12 cases), which could not be ascertained as malignant based on the histopathological features of the specimen alone.
Immunohistochemical analysis was done using two basal epithelial markers namely, p63 and high molecular weight cytokeratin (34beta E12), and one prostate-specific malignant cell marker, Alpha Methyl Acyl CoA Racemase (AMACR). As we did not have any financial assistance, the application of triple immunomarkers on each and every case possibly would cost high. Therefore immunomarkers were applied judiciously on 50 selected cases so that they covered all the suspicious cases, and only those cases were selected from the rest of the categories that either have atypical foci or mimickers, which could further improve our existing knowledge regarding cocktail immunomarkers in prostatic lesions.
Sections for Immunohistochemical assay were taken on poly-L-lysine coated clean glass slides. Endogenous peroxidase activity was blocked by freshly prepared 0.3% hydrogen peroxide in methanol for 15 min. Subsequently, heat‑induced antigen retrieval was performed as per manufacturers’ instructions. Immunohistochemistry (IHC) was performed by using a primary antibody (Thermo Scientific Anti-p63 Ab-1 clone 4A4 mouse monoclonal antibody; Ig class: IgG2a/κ) for the detection of p63. For HMWCK, primary antibody (Thermo Scientific Keratin, HMW Ab-3 clone 34βE12 mouse monoclonal antibody; Ig class: IgG1) was used, and for the detection of AMACR, primary antibody (Thermo Scientific p504S/ AMACR clone 13H4 rabbit monoclonal antibody; Ig class: IgG) was used. Diaminobenzidine (DAB) was used as chromogen in all cases.
For p63 and HMWCK, positive control was skin or squamous cell carcinoma and negative control was a case of Carcinoma Prostate. For AMACR, positive control was cortical cells of the kidney and negative control was Benign Prostatic Hyperplasia (BPH).
p63 showed nuclear positivity while HMWCK showed cytoplasmic positivity in basal cells in the benign glands and High-grade Prostatic Intraepithelial Neoplasia (HGPIN) glands. On the other hand, AMACR typically showed circumferential or cytoplasmic finely granular staining in the secretory epithelial cells in prostate cancer and HGPIN glands. The immunoexpression observed in various cases was categorized as weak (1+), moderate (+2), and strong (+3) on the basis of the intensity of staining obtained.
Statistical analysis was done between multiple groups using the Chi‑square test and Fisher exact test whichever was appropriate.
To calculate the specificity and sensitivity of triple immunomarkers p63, HMWCK, and AMACR in prostatic lesions, cases were clubbed together into two main categories and designated as follows: (1) all non-malignant cases and (2) malignant cases. Specificity and sensitivity for malignant vs non–malignant cases were calculated as follows:
Specificity = True-Negative Results/True-Negative Results+False-Positive Results
Sensitivity = True-Positive Results/True-Positive Results+False-Negative Results
The designations true and false are based on assumptions that p63 and HMWK are expressed in all non-malignant lesions but not in malignant cases. Similarly, for AMACR, true and false are based on the assumption that it is positive in malignant cases and negative in non-malignant cases.
Results
A total of 108 cases, comprising of 25 histopathologically proven cases of prostatic adenocarcinoma, 52 cases of benign prostatic lesions like BPH, 19 cases of premalignant and 12 cases with suspicious foci, formed part of the study group (n = 108). For the purpose of immunostaining, 8 cases were selected from the benign group (benign controls), 18 cases from the malignant group (malignant controls), 12 cases of premalignant lesions along all the 12 cases from the suspicious category were selected. Results for p63, HMWCK, and AMACR immunostaining in relation to the final diagnosis are shown in Table 1. The triple immunostain p63, HMWCK and AMACR assay performed on tissue sections produced consistent immunostaining results and was a reliable tool for the evaluation of problematic prostate foci in all types of prostate specimens.
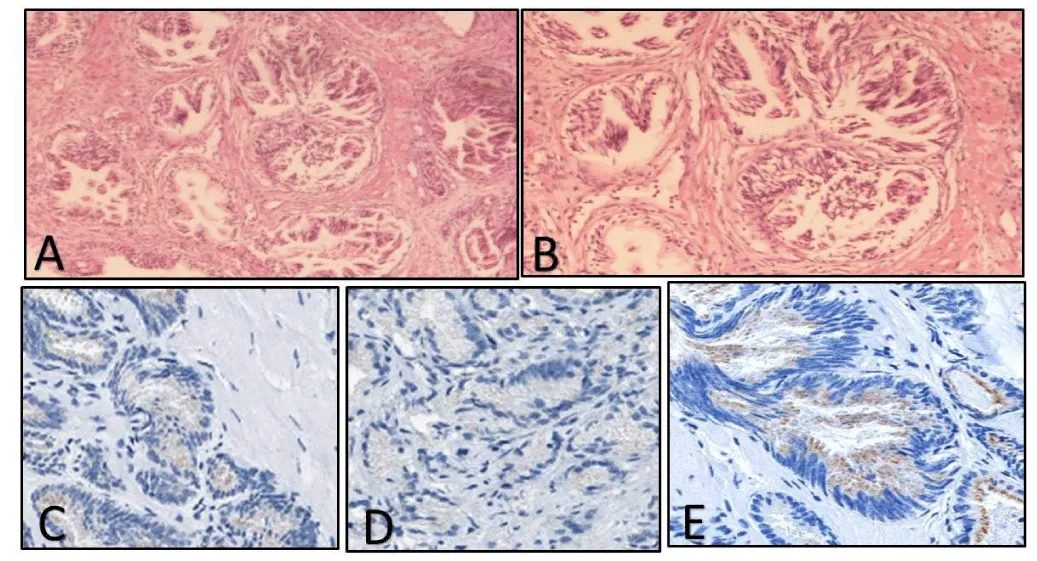
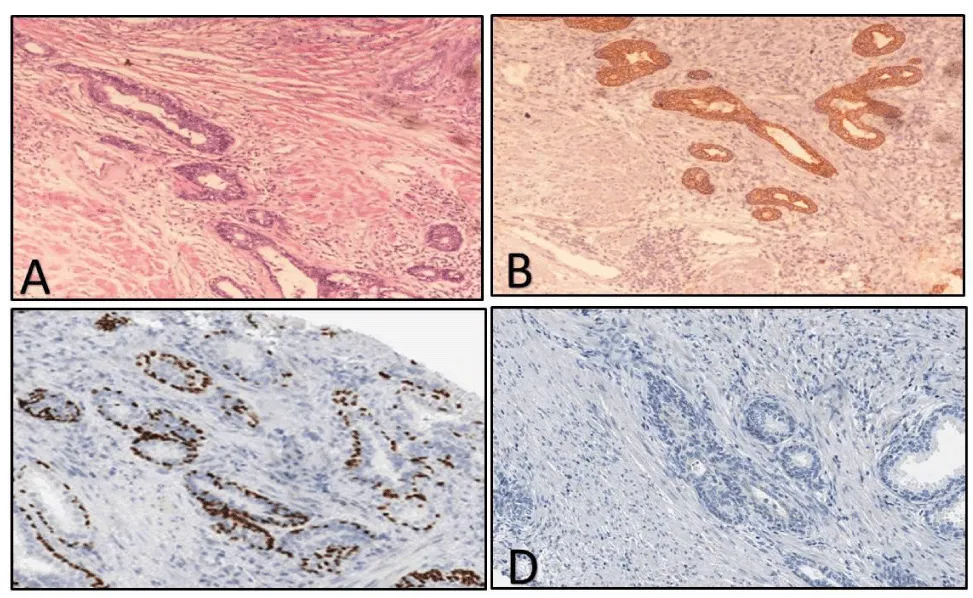
The cases of Group 4 showed either a few broken or fused glands amidst benign-appearing glands. These glands had cells with mildly atypical cytological or nuclear features consistent with atypical small acinar proliferation (ASAP) and were insufficient to diagnose them as malignant (Figure 1). Previous literature regarding mimickers of adenocarcinoma prostate made us aware and vigilant to not diagnose benign glands as malignant.
Result of immunohistochemistry
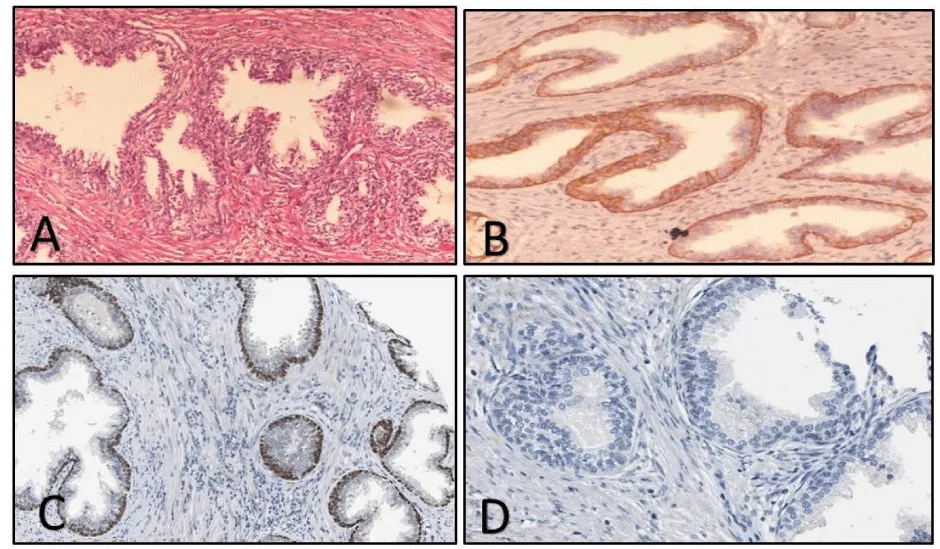
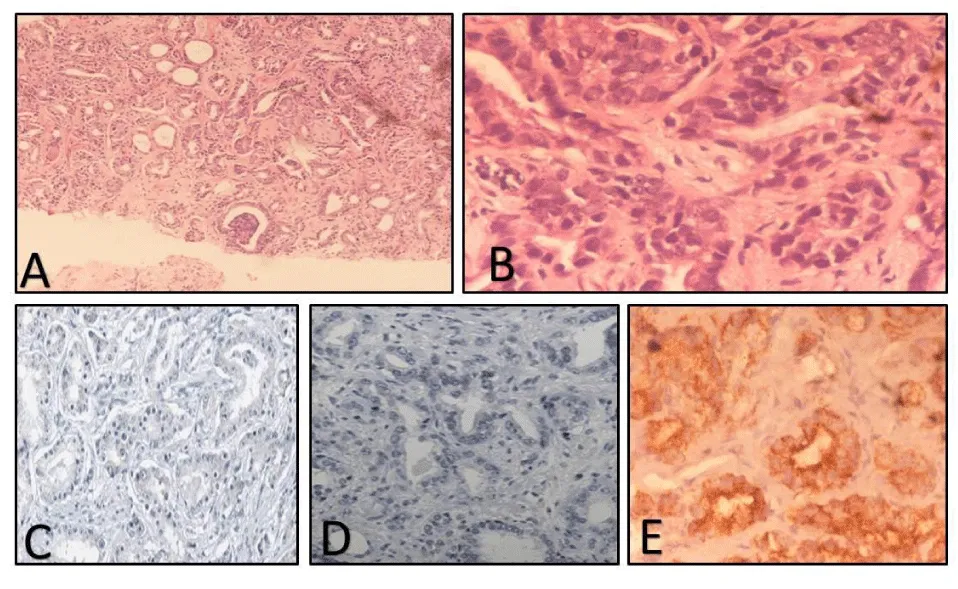
<p63: All the benign cases in Group 1 were positive for p63 basal cell marker showing strong nuclear positivity (Figure 2), except for 1 case of pure BPH which showed negative staining for p63. Amongst the premalignant group, 9 cases showed positive immunoreactivity of variable grades, while 1 case of Low-grade Prostatic Intraepithelial Neoplasia (LGPIN) and 2 cases of HGPIN were negative. In the malignant category, all 18 cases showed negative p63 immunostaining (Figure 3). Out of 12 suspicious cases, 8 cases (66.7%) were negative and 3 cases (25%) were weakly positive for p63 immunostaining. 1 case showed moderate staining (Table 1).
HMWCK: As seen in Table 1, all the benign cases in Group 1 were reactive for HMWCK showing moderate to strong positivity (Figure 2). Amongst the premalignant group, weak to moderate cytoplasmic positivity was seen except for 2 cases of HGPIN, which were negative. In the malignant category, all cases showed negative HMWCK immunoreactivity. Out of 12 suspicious cases, 7 cases (58.33%) were completely negative, 3 cases (25%) showed weak positivity, 1 case showed moderate and 1 case showed strong positivity for HMWCK (Table 1).
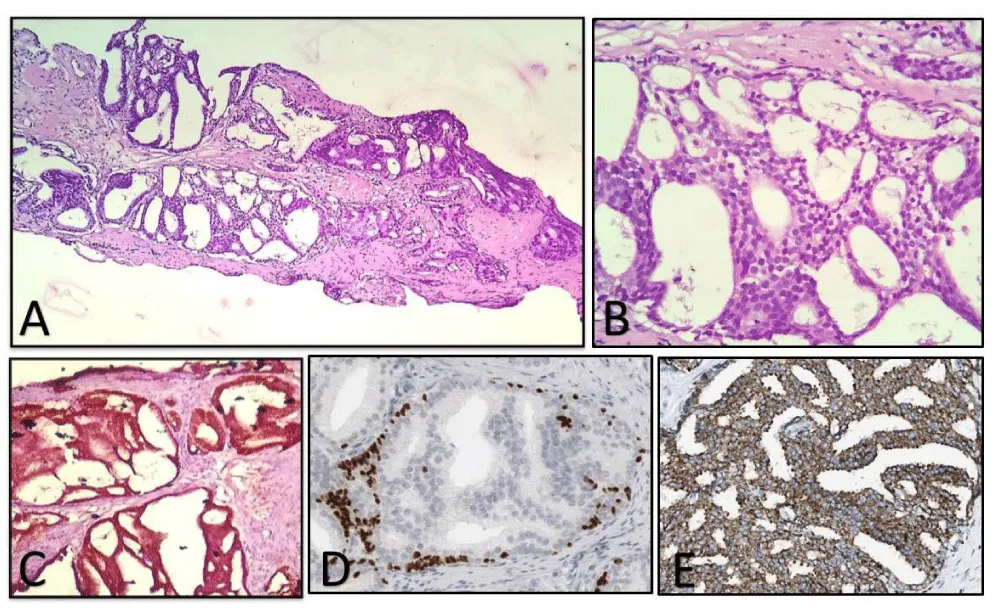
AMACR: All the benign cases in Group 1 were negative for AMACR. Amongst the premalignant group, 1 case (20%) of LGPIN and 3 cases (60%) of HGPIN showed positive immunoreactivity (Figure 4). In the malignant category, 15 out of 18 cases showed positive immunostaining (Figure 3). Three malignant cases that were negative corresponded with poorly differentiated adenocarcinoma with a Gleason Score of 9-10 on histomorphology (Table 1).
On assessing the grade of immunoreactivity in the malignant group, 13 cases showed moderate to strong immunostaining and 2 cases, which were foamy gland variants of adenocarcinoma, showed weak immunoreactivity. All four cases, which stained positive in the premalignant group, exhibited mostly weak and focal positivity. Out of 12 suspicious cases, 5 were negative and 7 were positive mostly showing moderate to strong positivity. Overall, in prostate carcinoma and HGPIN, AMACR was diffusely or focally positive in 15 of 18 and 3 of 5 cases, respectively (Figure 4). AMACR intensity was graded moderate (2+) to strong (3+) in 13 of 18 and 1 out of 5 cases in prostate cancer and HGPIN, respectively. HMWCK and p63 exhibited excellent specificity for prostate cancer, which uniformly lacked basal cell staining (100% negative). Thus the immunohistochemical panel of p63, HMWCK, and AMACR aided in resolving 10/12 (83.33%) suspicious cases and helped us in reaching a definite diagnosis in the majority of them (Table 1).
Statistical evaluation of immunohistochemical stains
On performing the statistical analysis of immunoexpression in diagnosing prostatic lesions, we found that p63 had a sensitivity of 80%, Whereas HMWCK had a sensitivity of 92%. Also, the specificity and positive predictive value of both p63 and HMWCK was 100%. The negative predictive value was seen to be 82.14% and 92% respectively for p63 and HMWCK respectively. Overall, it was found that p63 and HMWCK are statistically significant immunomarker in categorizing the lesions in the benign group having a p-value of <0.05 by Fisher exact probability test.
When statistical analysis of AMACR immunoexpression was done, it was seen that AMACR had a sensitivity of 86.96% and specificity of 76%. Also, positive predictive value and negative predictive value were seen to be 76.92% and 79.16% respectively. Overall, it was found to be a statistically significant immunomarker in classifying the lesions in the malignant group, having a p-value of <0.05 by Fisher exact probability test.
Evaluation of suspicious cases
Immunostaining by triple markers viz. p63, HMWCK and AMACR were performed on all the 12 cases of Group 4 wherein the diagnosis could not be ascertained based on histopathology alone and was earlier reported as suspicious. All these cases were re-evaluated using all the 3 immunomarkers and based on it, 3 of them were diagnosed as benign (Figure 5), 2 as HGPIN, 5 as malignant (Figure 1). Two cases were still left in the suspicious group and could not be categorized in either of the above three groups owing to the fact that all the three immunomarkers i.e. p63, HMWCK, and AMACR were negative.
Discussion
Prostatic needle biopsies constituted the most commonly encountered sample, (64.5%) followed by TURP comprising of 23.1% cases and few (12.4%) prostatectomy specimens, similar to studies done by Shah, et al. (2002) and Kumaresan, et al. (2010), reported 87.3% and 56.9% needle biopsies respectively [3,4].
BPH was the most common individual diagnosis with 48.14% of cases in our study. Xess, et al. (2001) and Ojewola, et al. (2013) also found comparable results with 42.8% and 58.6% incidence of benign prostatic diseases respectively [5,6].
In invasive prostate adenocarcinoma, the basal cell layer is absent, so a complete absence of staining of basal cell-associated immunomarker is supportive of a malignant transformation. Under routine hematoxylin-eosin (H&E) microscopy, basal cells may be mimicked by prostatic stromal cells adjacent to the glandular-basement membrane, by endothelial cells of blood vessels in close proximity to acini, and by tangentially sectioned neoplastic cells. The use of basal cell-associated markers helps in highlighting the basal cells present in benign prostate glands which have architecturally atypical, proliferations and mimic malignancy. However, sometimes there may be false negativity in basal cells of benign lesions or false positivity in malignancy. Studies showed that in 5% to 23% of cases, scattered, frankly, benign glands may show absent staining [7]. Staining may be weak-reactive to nonreactive in some benign lesions that simulate cancer, such as in up to 23% cases of glandular atrophy, up to 50% of atypical adenomatous hyperplasia (AAH; adenosis), and 23% cases of post–atrophic hyperplasia [7,8]. The prostate carcinoma-associated immunomarker, AMACR positivity supplements the lack of basal cell-associated staining in prostate carcinoma and thus helps the pathologists from false negativity associated with basal cell-related markers. Currently, AMACR is more commonly applied in association with basal cell markers in an antibody cocktail for diagnostic assessment of suspicious foci in prostate specimens. Jiang and co-workers also used a triple-antibody cocktail (containing antibodies to AMACR, HMWCK 34βE12, and p63) to identify small, focal prostate carcinomas with high sensitivity and complete specificity [9]. The use of triple immunoassay has increased pathologists’ certainty in establishing a definitive diagnosis.
In our study, we also used these immunomarkers sequentially on separate slides. The final diagnosis of malignancy was based on the combined use of cytoplasmic AMACR as a positive marker and basal cell marker p63 and HMWCK as negative. Molinie, et al. (2004) in their study used the p63-AMACR cocktail in resolving suspicious foci on prostatic needle biopsies. These cases were re-diagnosed as minimal focus cancers in 47%, benign lesions in 25%, high-grade prostatic intraepithelial neoplasia or atypical adenomatous hyperplasia in 17% and the remaining 11% were retained as persistent atypical small acinar proliferations with a suspected but unconfirmed diagnosis of malignancy [10]. Kumaresan, et al. (2010) demonstrated a change in 17 out of the 50 cases (34%) of suspicious cases, which was statistically significant [4]. In our study, the use of a combined IHC panel of p63, AMACR, and HMWCK aided in resolving 10/12 (83.33%) suspicious cases (Table 1). This change in the diagnosis before and after the application of immunohistochemistry was found to be statistically significant (p-value <0.05) similar to that seen by Singh, et al. (2014) [11]. They observed that in 11 cases (11/40), the diagnosis was changed from benign to malignant, and this change was statistically significant with a p-value of 0.013.
Conclusion
We observed that p63 and HMWCK had a high specificity for benign glands and AMACR had a high sensitivity for malignant glands. Also, based on the conclusions drawn from previous studies, we believe that, in a simple assay, the association of the antibodies, as a positive marker and the other as a negative marker, greatly facilitates the identification of various prostatic lesions, leading to a decrease in the risk of false negatives, an increase in diagnostic precision with improved sensitivity and specificity, especially in small needle biopsies.
The authors would like to thank the histology laboratory of the Department of Pathology, JNMC, AMU, Aligarh for technical expertise in performing the immunohistochemical stains.
Ethics approval
Informed consent was taken from each patient. The letter of approval and clearance was obtained from the Institutional Ethics Committee, JNMCH, AMU, Aligarh.
- Quinn M, Babb P (2002) Patterns and trends in prostate cancer incidence, survival, prevalence and mortality. Part I: international comparisons. BJU Int 90: 162-173. Link: https://bit.ly/3JhTVsP
- Ferlay J, Shin HR, Bray F, Mathers C, Parkin DM (2010) GLOBOCAN 2008, Cancer incidence and mortality worldwide: IARC Cancer Base No. 10. Lyon, France: International Agency for Research on Cancer. Link: https://bit.ly/3szhE0Y
- Shah RB, Zhou M, LeBlanc M, Snyder M, Rubin MA (2002) Comparison of the basal cell-specific markers, 34betaE12 and p63, in the diagnosis of prostate cancer. Am J Surg Pathol 26: 1161-1168. Link: https://bit.ly/3sqwKFW
- Kumaresan K, Kakkar N, Verma A, Mandal AK, Singh SK, et al. (2010) Diagnostic utility of α-methylacyl CoA racemase (P504S) & HMWCK in morphologically difficult prostate cancer. Diagn Pathol 5: 83. Link: https://bit.ly/3rEPsuj
- Xess A, Singh M, Raghwendra KH, Sharma HP, Shahi SK (2001) Prostate specific antigen as tumor marker: relationship with histologic grading. Indian J Pathol Microbiol 44: 261-264. Link: https://bit.ly/36av4sR
- Ojewola RW, Jeje EA, Tijani KH, Ogunjimi MA, Anunobi CC (2013) Clinico-pathological correlation of digital rectal examination findings amongst Nigerian men with prostatic diseases: A prospective study of 236 cases. Niger J Surg 19: 26-31. Link: https://bit.ly/3Jq0s4V
- Hameed O, Humphrey PA (2005) Immunohistochemistry in diagnostic surgical pathology of the prostate. Semin Diagn Pathol 22: 88-104. Link: https://bit.ly/3uIdN4q
- Amin MB, Tamboli P, Varma M, Srigley JR (1999) Postatrophic hyperplasia of the prostate gland: a detailed analysis of its morphology in needle biopsy specimens. Am J Surg Pathol 23: 925-931. Link: https://bit.ly/3gG6HoS
- Jiang Z, Li C, Fischer A, Dresser K, Woda BA (2005) Using an AMACR (P504S)/34betaE12/p63 cocktail for the detection of small focal prostate carcinoma in needle biopsy specimens. Am J Clin Pathol 123: 231-236. Link: https://bit.ly/3HQ5lUw
- Molinie V, Herve JM, Lebret T, Lugagne-Delpon PM, Saporta F, et al. (2004) Value of the antibody cocktail anti p63+ anti p504s for the diagnosis of prostatic cancer. Ann Pathol 24: 6-16. Link: https://bit.ly/3rFB8S5
- Singh V, Manu V, Malik A, Dutta V, Mani NS, et al. (2014) Diagnostic utility of p63 and α-methyl acyl Co A racemase in resolving suspicious foci in prostatic needle biopsy and transurethral resection of prostate specimens. J Can Res Ther 10: 686-692. Link: https://bit.ly/3sxaIl1
Article Alerts
Subscribe to our articles alerts and stay tuned.
 This work is licensed under a Creative Commons Attribution 4.0 International License.
This work is licensed under a Creative Commons Attribution 4.0 International License.
 Save to Mendeley
Save to Mendeley
