Journal of Novel Physiotherapy and Physical Rehabilitation
Virtual reality training and pain neuroscience plus motor control on pain, disability, health, and quality of life of women with non-specific chronic back pain
Ensiye Reza1*, Rafael Oliveira2-4, Behrooz Sarvari Far5, Faeze Molaee6 and Hadi Mohammadi Nia Samakosh7
2Sports Science School of Rio Maior–Polytechnic Institute of Santarém, 2040-413, Rio Maior, Portugal
3Life Quality Research Centre, 2040-413, Rio Maior, Portugal
4Research Center in Sport Sciences, Health Sciences and Human Development, 5001-801 Vila Real, Portugal
5Department of Physical Education and Sports Sciences, Islamic Azad University-East Tehran Branch, 5157944533, Tehran, Iran
6Department of Exercise Physiology, Sports Science faculty, Alzahra University, 1993891176 Tehran, Iran
7Department of Biomechanics and Corrective Exercises and Sports Injuries, University of Kharazmi, 15719-14911, Tehran, Iran
Cite this as
Reza E, Oliveira R, Far BS, Molaee F, Nia Samakosh HM (2024) Virtual reality training and pain neuroscience plus motor control on pain, disability, health, and quality of life of women with non-specific chronic back pain. J Nov Physiother Phys Rehabil 11(1): 001-010. DOI: 10.17352/2455-5487.000103Copyright
© 2024 Reza E, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.Background: Non-specific chronic low back pain is defined as a complex disorder involving structural, biomechanical, cognitive, psychological, social, and lifestyle factors. This randomized clinical trial study compared the effects of 8-week Virtual Reality Training (VRT) and pain neuroscience plus motor control training (PNE/MCT) on pain, disability, health, and quality of life of women with non-specific chronic back pain.
Methodology: This research is a single-center parallel RCT. Thirty-six participants participated in this study. They were divided into two groups: VRT (G1) and PNE/MCT (G2), both with 18 women. The training was performed for eight weeks for 45 minutes – 60 minutes. The VRT was applied by Oculus Quest 2. Visual Analogue Scale (VAS), disability (Oswestry Disability Index), general health (GHQ-28), and quality of life (QOL- WHO) were assessed before and after eight training weeks using a within-between group analysis (ANOVA 2×2).
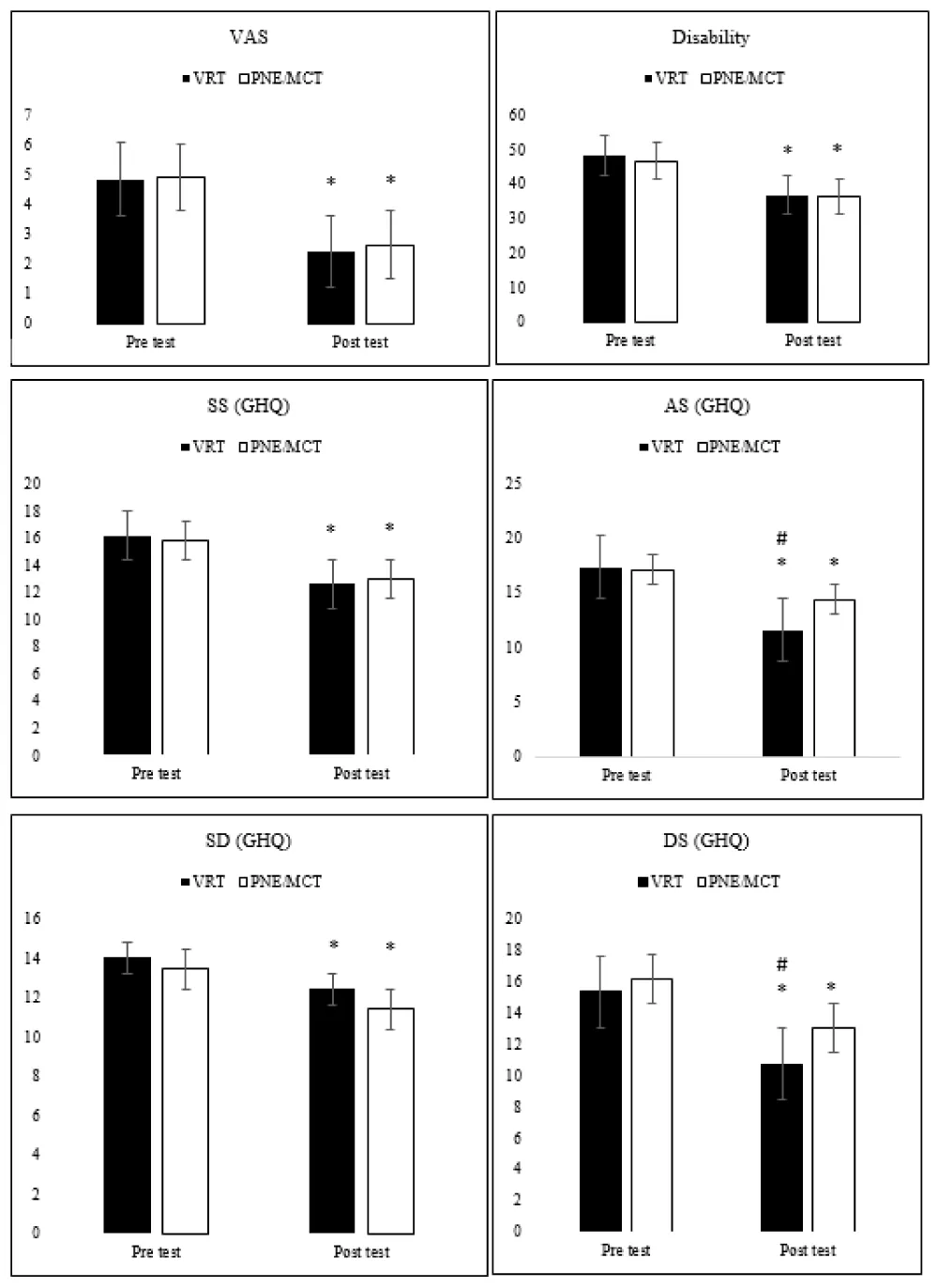
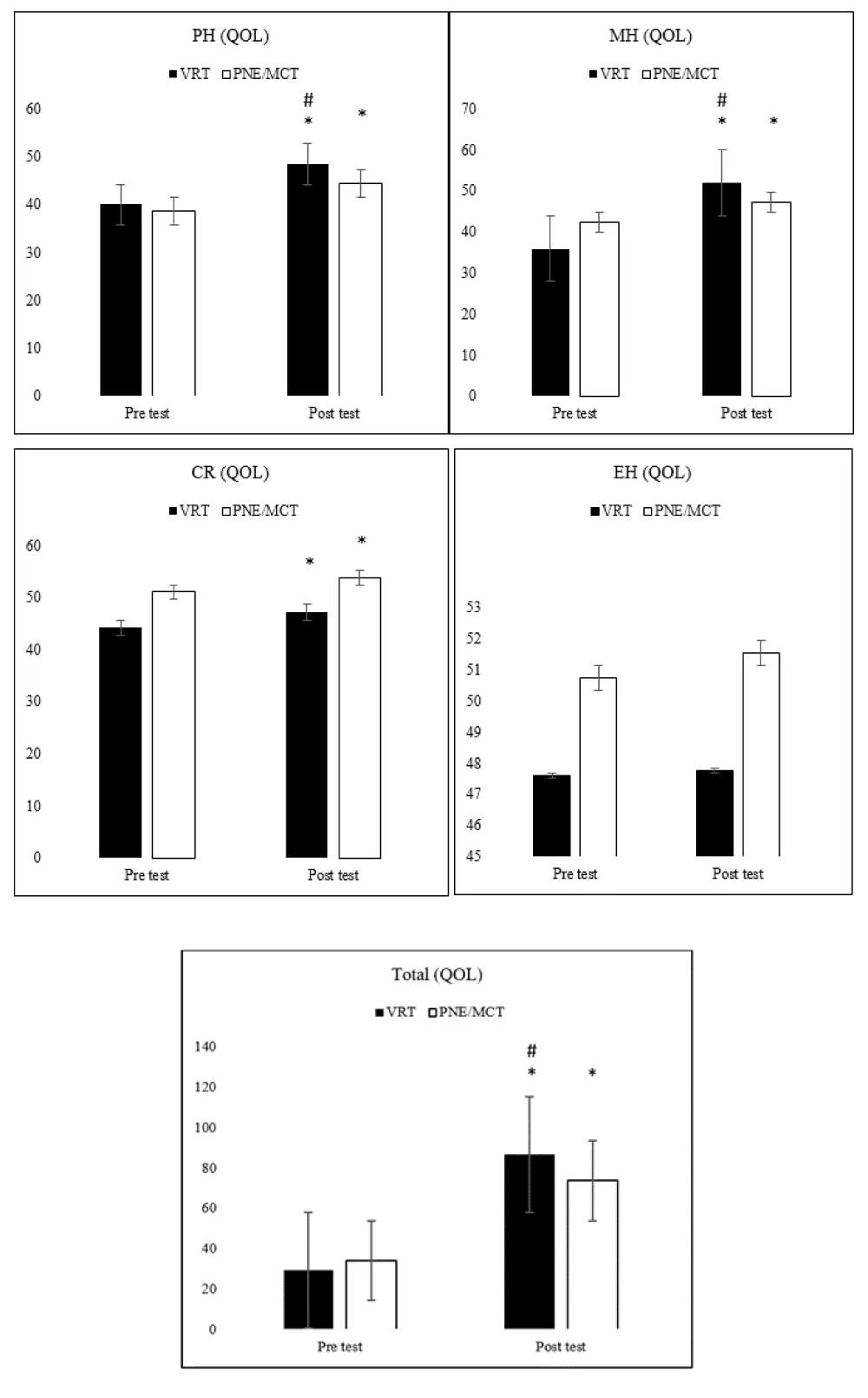
Results: Before training, no difference was observed between the groups (p > 0.05). After the intervention, both groups improved VAS, disability, GHQ, and QOL (all p < 0.001). In the comparison between the groups, the G1 had a better performance according to the p-value and effect size in anxiety (p = 0.001, ES= 0.71), depression symptoms (p = 0.03, ES: 0.25), physical health (p = 0.03, ES: -0.24), mental health (p = 0.001, ES: 0.66), and total QOL (p = 0.048, ES: 0.21) than G2.
Conclusion: Despite the effectiveness of both interventions, VRT improved the general health and quality of life in women with NSCLBP more than PNE/MCT.
Abbreviations
NSCLBP: Non-Specific Chronic Low Back Pain; PNE: Pain Neuroscience Education; MCT: Motor Control Training; VR: Virtual Reality; VAS: Visual Analog Scale; ODI: Oswestry Disability Index; GHQ: General Health Questionnaire; QOL: Quality of life; AS: Anxiety Symptoms; DS: Depression Symptoms; PH: Physical health; MH: Mental health; EH: Environmental Health; CR: Community Relationship
Introduction
Non-Specific Chronic Low Back Pain (NSCLBP) is a serious health problem in developed countries. Back pain can be classified based on the duration of the pain as well as the causes of the pain. Based on the duration, pain can be acute, subacute, or chronic. In the case of acute Low Back Pain (LBP), pain can last up to six weeks. In the case of subacute LBP, lumbosacral pain lasts from six to 12 weeks. Chronic LBP lasts for more than 12 weeks. Regarding the non-specific diagnosis of LBP, a clear cause can be defined in only 15% of cases [1,2].
The prevalence of chronic LBP among adults is 60% [1]. The prevalence of NSCLBP is strongly related to several social and demographic factors. It increases with age, being the most common musculoskeletal disorder among middle-aged adults. Women are more commonly affected than men because they present sedentary jobs or physically demanding jobs such as heavy lifting [3,4]. The prevalence of low back pain is 39% (35% in males, and 42% in females) [5]. Back pain is the leading cause of years of life with disability worldwide [6]. In addition, this problem has a significant impact on other social and economic aspects because in developed societies NSCLBP is the most common reason for leaving work [7]. Moreover, the financial burden caused by NSCLBP has a significant impact on the financing of the health care system [8-10]. For instance, Waxman et al. investigated the association between NSCLBP and depressive symptoms. Pain encourages the patient to cope with the disease, affecting the quality of life, and reducing life satisfaction [7]. It was also stated that mental health symptoms are strongly associated with NSCLBP. Evidence suggests that mental health symptoms are negative prognostic factors for NSCLBP [10,11]. People with mental health symptoms such as depression or anxiety symptoms show poorer recovery from NSCLBP [12]. Preliminary evidence suggests that symptoms of depression or anxiety are more common in patients with NSCLBP who use care [13].
In the context of factors affecting the development of back pain, the weakness of the multifidus muscles of the back can disrupt the function of the spine both during dynamic movements and in static positions. therefore, exercise protocols for NSCLBP aim to increase function through lumbar stability exercises that target the multifidus muscles [14]. In addition, more knowledge about spinal motor dysfunction in patients with NSCLBP has emerged [15]. Patients with NSCLBP who have decreased motor control usually have difficulty controlling postures and movements [15]. Therefore, dealing with pain diagnosis and better function of spinal muscles to improve spinal motor control can be more effective [16].
A method that included Pain Neuroscience Education (PNE) followed by Motor Control Training (MCT) has recently been used [16]. This method aims to teach the mechanisms of chronic LBP (central pain, central sensitization, and cognitive-sensory mechanisms of pain) followed by individual MCT to help patients develop activities they do with fear and hesitation [17]. In this regard, a study showed that a PNE program combined with motor control training with cognitive goals reduced pain and disability and increased spine function compared to physical therapy intervention in patients with chronic LBP. Furthermore, a recent systematic review and meta-analysis showed that exercise training programs achieved similar clinical effects compared to physical therapy interventions [18]. In this regard, Gorji, et al. showed that PNE/MCT was effective on pain, disability, and performance of women with chronic LBP, and PNE/MCT also performed better compared to core stability training [19].
In addition to this type of training, one emerging technology with the potential to influence chronic LBP that cannot be achieved by other means is Virtual Reality (VR) [20]. VR is a goal-based reality and simulation of computer games that allow changing people’s experience of their perceived world [21,22]. Rapid advances in technologies such as VR have shown promise for the treatment of a variety of diseases and disorders such as chronic pain.
Some recent reviews with meta-analyses have shown the usefulness and benefits of VR treatments in acute and chronic pain [23,24]. Research supports VR as a therapeutic strategy for both acute and chronic pain [24-26]. It has been suggested that the mechanism of action of VR is to influence activation in the anterior cingulate cortex and periaqueductal gray [27]. VR Training (VRT) has been gradually incorporated into rehabilitation training programs in patients with CNLBP and has been shown to reduce pain and improve functional impairment [28]. Yelfani, et al. showed that VRT can be considered a valid therapeutic intervention by teaching insight related to pain as well as increasing the quality of life and reducing the risk of falling through different methods to reduce the symptoms of patients and increase the effectiveness of exercises in the NSCLBP [29]. Also, they used the eight-week training to play Xbox games.
Based on the mentioned cases, the present study was conducted to compare VRT and PNE/MCT on pain, disability, health, and quality of life of women with NSCLBP. In this study, it was hypothesized that both training programs improved all research variables.
Material and methods
Experimental design
This study was conducted following the Consolidated Standards of Reporting Trials (CONSORT) guidelines [30] and our study is a single-center, double-blind randomized controlled trial. It was adopted as a design of a two-group study presented in two experimental groups with equal randomization (1:1): VRT and PNE/MCT. Both interventions lasted eight weeks.
The present study was registered and approved by the ethics committee of the Polytechnic Institute of Santarém (29-2022ESDRM) and was prospectively registered in the clinical trial registry (UMIN000049808). RTC Link: https://center6.umin.ac.jp/cgi-open bin/ctr_e/ctr_view.cgi?recptno=R000056720.
Participants recruitment and eligibility criteria and randomization
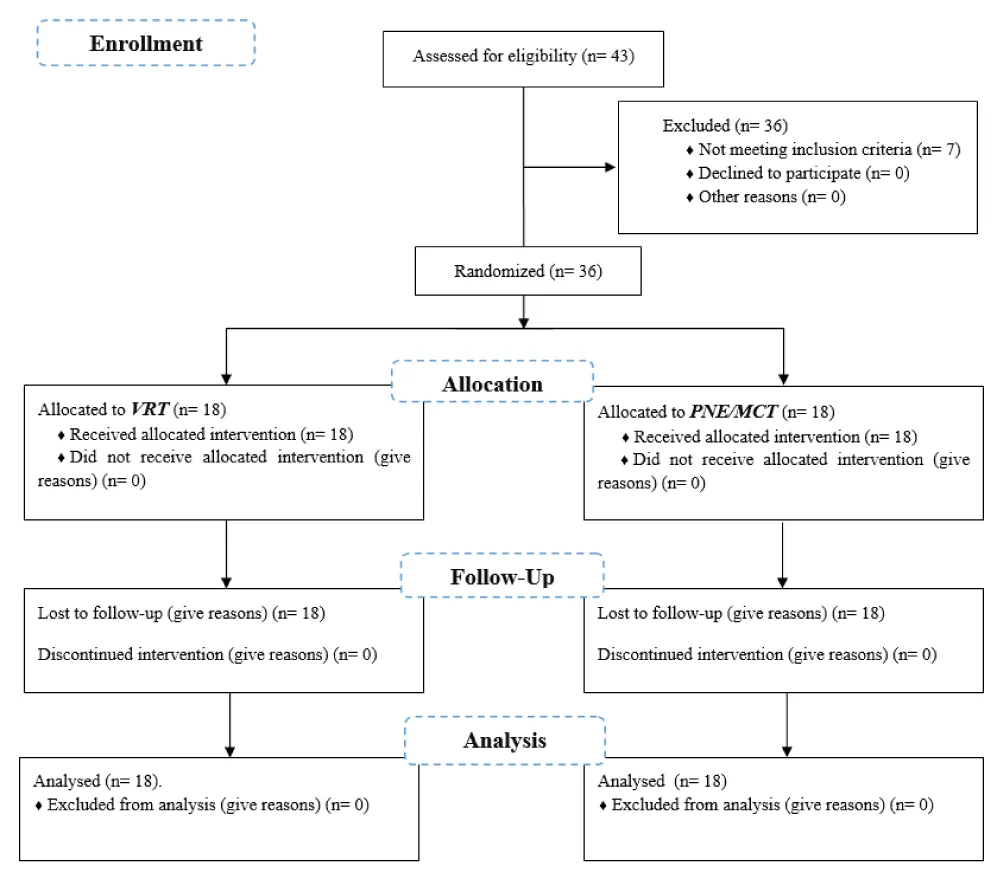
In this study, among 43 eligible women with NSCLBP, 36 were selected according to the entry criteria and willingness to cooperate until the end of the process. We considered women who visited the Media Physiotherapy Clinic in Tehran (Iran). They were divided into two groups: VRT; n: 18, age: 31.11 ± 7.84 yr, height: 1.66 ± 0.02 m, weight: 58.83 ± 3.03 kg. PNE/MCT; n: 18, age: 33.00 ± 8.39 yr, height: 1.68 ± 0.03 m, weight: 59.55 ± 4.63 kg. Telescopic height measuring model-MZ10023-3 (ADE, Hamburg, Germany), was used to evaluate height and weight, weight was assessed in the morning when the patient’s bladder was empty and wearing light clothes [31].
The following eligibility criteria were applied:
- Inclusion criteria: (1) women age range between 20 years - 45 years; (2) average pain level ≥ 4 on a 10-cm Visual Analog Scale (VAS) during the Straight Leg Raise test [32] and (3) reporting pain in the last six months.
- Exclusion criteria: (1) any history of back surgery; (2) having orthopedic and neurological injuries; (4) reporting of pain in the buttock to back during training, and (5) medication as part of treatment [33]. Participants were also excluded if they were undergoing other types of therapy, specific work activities, or regular treatments (such as stretching, taping, braces, orthotics, and/or acupuncture) or if they failed two consecutive sessions or the post-test phase.
Randomization
Participants were informed of the risks and benefits of the study before collecting data. Then, participants signed an informed consent form according to the Helsinki Declaration [34]. Finally, and before randomization, descriptive social data and initial clinical outcome variables were collected from all participants.
A double-blind randomized clinical trial was used. The term double-blind (masking) refers to the fact that both the researcher and participants did not know which group the participants were allocated to. The advantage of this blinding is twofold: the researcher cannot affect the outcome of the study by treating participants in the intervention groups differently and the participants are not influenced by knowing whether they received the training, a blinded person (not the researcher) generated the allocation sequence, and one other person as trainer enrolled participants and assigned them to interventions. Also, the allocation sequence was concealed until participants were enrolled and assigned to interventions. Participants were assigned to one of two treatment groups, with equal randomization (ratio of 1:1). Randomization was performed by a blinded person who did not know the aims or design of the study. Randomization was performed with each person-specific naming code (up to 36) previously sealed in an envelope: the blind person was asked to place 18 cards in both balls.
Interventions
Before the interventions, the participants executed a standardized 5-min warm-up protocol consisting of a series of double leg squats (2 × 8 repetitions) and double leg maximum jumps (2 × 5 repetitions), followed by dynamic calf-stretching with a straight and bent knee [35].
VRT: The G1 received 24 sessions within eight weeks (three times a week) with a VR headset model; Oculus Quest 2 (Facebook Technologies Ltd., Menlo Park, CA, USA). The games used in this study are from three packages: PowerBeats, Swords of Gargantua, and VR-Workout. VR-Workout is a fitness rhythm game with full-body engagement including Jumping / Squatting / Pushups / Side Planks / Crunches / standing on single leg / Burpees and Sprinting exercises. The intensity of the games was from easy to hard according to the Rated Perceived Exertion (RPE) scale (10 – 15 points in the Category-Ratio (CR) 20) provided [36]. This scale numerically ranges from 6 to 20, where 6 means “no exertion at all” and 20 means maximal exertion [36], and is based on the ability and progress of each participant in doing each step of the game.
Each training session lasted about 30 min - 45 min, in which the person performed 5 min of warm-up before the game, 5 min of cooling after the game, and 20 min - 35 min of practice with Oculus Quest 2. The participants could play freely and move their whole body in the space with KinectTM (Microsoft, Redmond, WA, USA) [37,38].
Participants were trained to familiarize themselves with the practice by showing them video clips of the model and allowing them to attempt practice in three sessions while playing games and training with individuals as physical therapists with more than seven years of experience monitoring their performance. After mastering the exercises related to the VR-Workout game, they were allowed to perform each exercise for 10-15 repetitions in 3 sets. Rest was 30 seconds between each set and 60 seconds between each exercise. The intensity of the training was adjusted based on the individual’s ability, as well as the principle of overload during the eight weeks of training, so that the duration of the game, the number of sets in the training, and the number of repetitions were added.
PNE/MCT: Three PNE sessions had 30 minutes - 60 minutes and were conducted by a physical therapist. The purpose of the PNE was to control patients’ negative perceptions of recurring pain [39,40]. These beliefs may be imposed on patients by potentially useless diagnostic, prognostic, or therapeutic conclusions. During the PNE sessions, pain information was given to avoid fear beliefs and behaviors, thus providing keywords at this stage to promote self-efficacy using verbal instructions, charts, and freehand drawings [39,40].
The MCT was similar to Malfliet, et al. [39]. Training and treatment fidelity methods in the PNE/MCT group are described in the published protocol [19]. Table 1 presents MCT.
Outcomes
An assessor, blinded to the allocation of the group participants, to the research aims and design, performed the assessments. The following primary and secondary outcomes were applied to all participants.
Primary outcomes
- The Visual Analog Scale (VAS) was used to measure the participants’ pain severity. The scale is a 10 cm horizontal strip starting from 0 (no pain) to 10 (the most severe pain possible). This scale is one of the most reliable quantitative scales widely used in research [19], reliability of the VAS is (ICC = 0.99) [41].
- The Oswestry Disability Index (ODI) was used to measure the participants’ disability severity. ODI consists of 10 items on the degree of severity to which back (or leg) trouble has affected the ability to manage in everyday life [42]. The 10 sections cover the pain and the daily function (including pain intensity, personal hygiene, lifting, walking, sitting, standing, sleeping, sexual activity, social activity, and traveling). Each item is rated on a 6-point scale (0 – 5); the higher score means the higher level of disability related to LBP. The present study used the traditional version of the ODI [43]. ODI Reliability is (ICC = 0.89 – 98) [44].
Secondary outcomes
- The General Health Questionnaire (GHQ-28) was used to measure the participants’ general health. The questionnaire was presented by Goldberg and Hiller [45]. In addition to questions on personal and social characteristics, this questionnaire has four areas: physical symptoms, anxiety symptoms, social dysfunction, and depression symptoms. Each area has 7 items. The scale of the 4-point questionnaire is not at all (with a score of zero), in the normal range (score 1), it is more than usual (score 2) and much more than usual (score 3). The range of scores for each area is 0 - 21 and the range of the total score of the questionnaire is 0-84. The higher the person’s score, the less general health, and the lower the score, the more general health [46]. Its reliability is moderate (ICC = 0.78) [47].
- The Quality of life (QOL- WHO) was used to measure the participants’ quality of life. Quality of life was measured using the short form of the World Health Organization quality of life questionnaire. This questionnaire has 26 questions and measures the quality of life in four physical, psychological, social, and environmental dimensions. This standard questionnaire is extracted from the version of 100 questions. Hundreds of prominent researchers and dozens of official World Health Organizations from different countries have contributed to its production and standardization in 19 different languages [45]. The Persian version was used in this study [48]. High test-retest reliability was found for this Questionnaire (ICC = 0.98) [49].
Statistical analysis
The Shapiro–Wilk test and Levene’s tests were conducted to confirm the normality and homogeneity of the dependent variables, respectively. After both were confirmed, a 2 × 2 ANOVA (treatment group × time) with Bonferroni correction post hoc was conducted with a mixed model analysis design. Mean ± standard deviation (SD) was used for each dependent variable. The percentage of change was also calculated. A p - value < 0.05 was used to determine statistical significance, while Partial Eta Squared (ηp2) values were calculated as effect size (ES), which was considered 0.01 = small effect, 0.06 = moderate effect, and 0.14 = large effect, based on the study of Cohen [50]. Data analyses were conducted on SPSS software version 26 (IBM Corp., Armonk, NY, USA).
Sample size
The sample power of the post hoc F-test family (Repeated Measures Anova with within - between interaction) was calculated for α level = 0.05; effect size = 0.25; two groups, two measurements, and n = 36 by the G-Power [51]. It was shown that there was an 83% (actual power) for the analysis.
Results
Participants
Thirty-six women with NSCLBP ages 20 to 45. For each group, 18 women were allocated. These were women who reported NSCLBP (Figure 1).
Baseline
Table 2 lists the general characteristics of the participants in the study. Baseline data of age, height, weight, Body Mass Index (BMI), and pain duration did not significantly differ (p > 0.05) between VR and PNE/MCE. In addition, there were no differences within groups.
Tables 3,4 present the analysis of the variance with a 2×2 ANOVA (treatment time × group) test that showed significant group interactions overtime for Anxiety symptoms (AS), Depression Symptoms (DS), Physical Health (PH), and Mental Health (MH), as well as the Total QOL variables (p ≤ 0.05). Baseline comparisons revealed no significant differences between groups at baseline testing for all variables.
Overall, both groups improved significantly between baseline and after eight weeks except for Environmental Health (EH) of QOL. On the other hand, in the between-groups comparison, the G1 scored better than the G2 in AS, DS, PH, and MH, as well as the Total QOL. For better understanding, Figures 2 and 3 show the results of VAS, disability, GHQ, and QOL between groups and between pre-test against post-test.
Discussion
The present study compared VRT and PNE/MCT on pain, disability, general health quality, and quality of life of women with NSCLBP. The results of VRT in the present study were in line with some studies. For instance, Mbada, et al. pointed out the effects of VRT on reducing the pain of back pain patients [52]. Alemanno, et al. showed the effects of VRT on reducing pain, improving quality of life, physical function, cognitive function, and social function as well as the mood of back pain [53]. Moreover, Gorji, et al. [19] and Wood and Hendrick demonstrated the effects of PNE on reducing pain and disability caused by NSCLBP were consistent [54].
Overall, after eight weeks of treatment, a significant reduction in pain scores was observed. This reduction in pain has also been associated with a reduction in disability. These data provide evidence that VRT can be effective in helping chronic LBP patients to recover better motor function along with reducing the feeling of pain, thereby improving their quality of life and general health. VR-related therapy was based on the hypothesis that helping patients regain correct body perception would help them to improve their functional abilities reduce their quality of life and pain perception and increase their general health quality. The fact that patients improved significantly in repeatability and range of motion with training seems to indicate that VR-based rehabilitation can significantly improve proprioception and function [54,55]. The results showed that this VRT can work on pain and aspects of multiple disabilities and general health. A combination of all these multidimensional aspects may be responsible for improvements in different sub-sectors of quality of life.
In the context of the effectiveness of PNE/MCT, a growing body of evidence shows that changes in brain abnormalities in brain structure and function and brain hypersensitivity in patients with chronic LBP are of major importance [17]. Central sensitization involves altered sensory processing in the brain [17]. Furthermore, brain plasticity causes pain and fatigue, which can lead to disability even without tissue damage or actual pain [17]. In this regard, the PNE/MCT offers significant improvements to combat these issues [39]. Central sensitivity was not evaluated in the present study. However, it has been hypothesized that educating patients on how to control pain and understand how they feel can help reduce central nervous system hypersensitivity and relieve pain [56-58]. This factor, along with performing motor control exercises may be a factor in the effectiveness of this exercise program on pain and disability. Physical feedback and cognitive biofeedback along with the implementation of exercise programs have been suggested in some studies to achieve better results in the elderly [59]. It seems that adding movement control training to neurological exercises by reducing pain and disability by activating proprioception, coordination and sensory-motor control of the spine helps patients in reducing disability and increasing their functional capacity can increase their general health. That has been found as a factor in improving the quality of life of these people [56-58].
In terms of the greater effect of VRT compared to PNE/MCT on variables such as the dimension of anxiety and depression related to the quality of general health, as well as physical and mental health and the overall quality of life score, it can be attributed to the characteristics of the VRT. The VRT was based on mobility due to the presence of movements such as jumping, squatting, and sprinting, which are presented as a game and can lead to more effects on some parameters of health quality due to attractiveness and physical and mental involvement, general health and quality of life compared to PNE/MCT. However, no other studies comparing the same protocols were found and for that reason, the replication of this study is required. Even so, it is relevant to highlight that this is the first study to compare VRT and PNE/MCT.
Considering that chronic pain has become a major health concern worldwide, pharmaceutical companies are currently treating chronic back pain through the development of drug formulations [60]. Furthermore, the development of alternative and non-pharmacological therapies is necessary to provide the best-personalized care to patients and reduce the risk of drug abuse. Non-pharmacological treatments can also show the benefit of good compliance among patients. In particular, VRT as well as PNE/MCT were reported as effective treatments in this research.
Conclusion
The main hypothesis of this study was confirmed because both interventions improved pain, disability, general health quality, and quality of life Specifically and according to the main effect (time), after eight weeks, both groups had an effect on all variables except environmental health. On the other hand, according to the main effect (group * time), the VRT showed significantly higher improvements in the variables of depression, anxiety, physical and mental health, and the total quality of life score compared to PNE/MCE. Nonetheless, both training programs seem to be recommended for women with NSCLBP.
Limitations and future directions
Despite the positive effects denoted by both interventions, some limitations should be listed such as only eight weeks were evaluated; the lack of a control group; and the lack of central sensitization assessment once there is no translated Persian version for this assessment. Therefore, future studies should consider longer longitudinal training protocols and the use of a control group, it can also occur between men and women at the same time. The next topic is the kinematic analysis of the lumbar region, which can be used in the future.
We wish to convey our heartfelt gratitude to the medical professionals and institution leadership from whom we sourced our participants. Additionally, we extend our warm appreciation to the individuals who generously volunteered to take part in this research.
- Járomi M, Szilágyi B, Velényi A, Leidecker E, Raposa BL, Hock M, Baumann P, Ács P, Makai A. Assessment of health-related quality of life and patient's knowledge in chronic non-specific low back pain. BMC Public Health. 2021 Apr 23;21(Suppl 1):1479. doi: 10.1186/s12889-020-09506-7. PMID: 33892680; PMCID: PMC8063275.
- Porter G, Omwega N. Experiences of Women Workers in the African Road Transport Sector, in Women, Work and Transport. Emerald Publishing Limited. 2022; 55-69.
- Ghafouri M, Teymourzadeh A, Nakhostin-Ansari A, Sepanlou SG, Dalvand S, Moradpour F, Bavarsad AH, Boogar SS, Dehghan M, Ostadrahimi A, Aghazadeh-Attari J, Kahnooji M, Hosseinipour A, Gohari A, Hosseini SV, Mirzaei M, Khorram A, Shahmoradi M, Pourfarzi F, Moosazadeh M, Mansour-Ghanaei F, Marioryad H, Najafi F, Genevay S, Moghadam N, Kordi R. Prevalence and predictors of low back pain among the Iranian population: Results from the Persian cohort study. Ann Med Surg (Lond). 2022 Jan 10;74:103243. doi: 10.1016/j.amsu.2022.103243. PMID: 35145656; PMCID: PMC8801351.
- Motuma A, Demissie Regassa L, Gobena T, Teji Roba K, Berhane Y, Worku A. Almost all working adults have at least one risk factor for non-communicable diseases: Survey of working adults in Eastern Ethiopia. PLoS One. 2022 Feb 28;17(2):e0264698. doi: 10.1371/journal.pone.0264698. PMID: 35226698; PMCID: PMC8884490.
- Papageorgiou AC, Croft PR, Ferry S, Jayson MI, Silman AJ. Estimating the prevalence of low back pain in the general population. Evidence from the South Manchester Back Pain Survey. Spine (Phila Pa 1976). 1995 Sep 1;20(17):1889-94. doi: 10.1097/00007632-199509000-00009. PMID: 8560337.
- Wong JJ, Côté P, Tricco AC, Watson T, Rosella LC. Joint effects of back pain and mental health conditions on healthcare utilization and costs in Ontario, Canada: a population-based cohort study. Pain. 2022 Oct 1;163(10):1892-1904. doi: 10.1097/j.pain.0000000000002587. Epub 2022 Jan 25. PMID: 35082249.
- Waxman SE, Tripp DA, Flamenbaum R. The mediating role of depression and negative partner responses in chronic low back pain and relationship satisfaction. J Pain. 2008 May;9(5):434-42. doi: 10.1016/j.jpain.2007.12.007. Epub 2008 Mar 3. PMID: 18313363.
- Ács P. Economic and public health benefits: the result of increased regular physical activity. European Journal of Integrative Medicine. 2016; 8: 8-12.
- Alsiddiky AM, Algarni N, Alluhaidan A. Prevalence and Associated Factors of Low Back Pain among Clinicians of A Major Referral Hospital. Med J Malaysia. 2015 Feb;70(1):12-7. PMID: 26032523.
- Ács P, Stocker M, Oláh A. The determination of economic and public health benefits achievable by increasing regular physical exercise. Applied studies in agribusiness and commerce. 2013; 7(1): 5-13.
- Pinheiro MB, Ferreira ML, Refshauge K, Maher CG, Ordoñana JR, Andrade TB, Tsathas A, Ferreira PH. Symptoms of depression as a prognostic factor for low back pain: a systematic review. Spine J. 2016 Jan 1;16(1):105-16. doi: 10.1016/j.spinee.2015.10.037. Epub 2015 Oct 30. PMID: 26523965.
- Wertli MM, Eugster R, Held U, Steurer J, Kofmehl R, Weiser S. Catastrophizing-a prognostic factor for outcome in patients with low back pain: a systematic review. Spine J. 2014 Nov 1;14(11):2639-57. doi: 10.1016/j.spinee.2014.03.003. Epub 2014 Mar 7. PMID: 24607845.
- Stewart WF, Yan X, Boscarino JA, Maeng DD, Mardekian J, Sanchez RJ, Von Korff MR. Patterns of health care utilization for low back pain. J Pain Res. 2015 Aug 12;8:523-35. doi: 10.2147/JPR.S83599. PMID: 26316803; PMCID: PMC4540213.
- Hides JA, Stanton WR, McMahon S, Sims K, Richardson CA. Effect of stabilization training on multifidus muscle cross-sectional area among young elite cricketers with low back pain. J Orthop Sports Phys Ther. 2008 Mar;38(3):101-8. doi: 10.2519/jospt.2008.2658. Epub 2007 Dec 7. PMID: 18349481.
- D'hooge R, Hodges P, Tsao H, Hall L, Macdonald D, Danneels L. Altered trunk muscle coordination during rapid trunk flexion in people in remission of recurrent low back pain. J Electromyogr Kinesiol. 2013 Feb;23(1):173-81. doi: 10.1016/j.jelekin.2012.09.003. Epub 2012 Oct 15. PMID: 23079004.
- Bodes Pardo G, Lluch Girbés E, Roussel NA, Gallego Izquierdo T, Jiménez Penick V, Pecos Martín D. Pain Neurophysiology Education and Therapeutic Exercise for Patients With Chronic Low Back Pain: A Single-Blind Randomized Controlled Trial. Arch Phys Med Rehabil. 2018 Feb;99(2):338-347. doi: 10.1016/j.apmr.2017.10.016. Epub 2017 Nov 11. PMID: 29138049.
- Nijs J, Meeus M, Cagnie B, Roussel NA, Dolphens M, Van Oosterwijck J, Danneels L. A modern neuroscience approach to chronic spinal pain: combining pain neuroscience education with cognition-targeted motor control training. Phys Ther. 2014 May;94(5):730-8. doi: 10.2522/ptj.20130258. Epub 2014 Jan 30. PMID: 24481595.
- O'Keeffe M, Hayes A, McCreesh K, Purtill H, O'Sullivan K. Are group-based and individual physiotherapy exercise programmes equally effective for musculoskeletal conditions? A systematic review and meta-analysis. Br J Sports Med. 2017 Jan;51(2):126-132. doi: 10.1136/bjsports-2015-095410. Epub 2016 Jun 24. PMID: 27343238.
- Gorji SM, Mohammadi Nia Samakosh H, Watt P, Henrique Marchetti P, Oliveira R. Pain Neuroscience Education and Motor Control Exercises versus Core Stability Exercises on Pain, Disability, and Balance in Women with Chronic Low Back Pain. Int J Environ Res Public Health. 2022 Feb 25;19(5):2694. doi: 10.3390/ijerph19052694. PMID: 35270384; PMCID: PMC8910692.
- Won AS, Bailey J, Bailenson J, Tataru C, Yoon IA, Golianu B. Immersive Virtual Reality for Pediatric Pain. Children (Basel). 2017 Jun 23;4(7):52. doi: 10.3390/children4070052. PMID: 28644422; PMCID: PMC5532544.
- Matsangidou M. Is your virtual self as sensational as your real? Virtual Reality: The effect of body consciousness on the experience of exercise sensations. Psychology of sport and exercise. 2019; 41: 218-224.
- Trost Z, Zielke M, Guck A, Nowlin L, Zakhidov D, France CR, Keefe F. The promise and challenge of virtual gaming technologies for chronic pain: the case of graded exposure for low back pain. Pain Manag. 2015;5(3):197-206. doi: 10.2217/pmt.15.6. PMID: 25971643.
- Matamala-Gomez M, Donegan T, Bottiroli S, Sandrini G, Sanchez-Vives MV, Tassorelli C. Immersive Virtual Reality and Virtual Embodiment for Pain Relief. Front Hum Neurosci. 2019 Aug 21;13:279. doi: 10.3389/fnhum.2019.00279. PMID: 31551731; PMCID: PMC6736618.
- Mallari B, Spaeth EK, Goh H, Boyd BS. Virtual reality as an analgesic for acute and chronic pain in adults: a systematic review and meta-analysis. J Pain Res. 2019 Jul 3;12:2053-2085. doi: 10.2147/JPR.S200498. PMID: 31308733; PMCID: PMC6613199.
- Carrougher GJ, Hoffman HG, Nakamura D, Lezotte D, Soltani M, Leahy L, Engrav LH, Patterson DR. The effect of virtual reality on pain and range of motion in adults with burn injuries. J Burn Care Res. 2009 Sep-Oct;30(5):785-91. doi: 10.1097/BCR.0b013e3181b485d3. PMID: 19692911; PMCID: PMC2880576.
- Schmitt YS, Hoffman HG, Blough DK, Patterson DR, Jensen MP, Soltani M, Carrougher GJ, Nakamura D, Sharar SR. A randomized, controlled trial of immersive virtual reality analgesia, during physical therapy for pediatric burns. Burns. 2011 Feb;37(1):61-8. doi: 10.1016/j.burns.2010.07.007. Epub 2010 Aug 7. PMID: 20692769; PMCID: PMC2980790.
- Gold JI, Belmont KA, Thomas DA. The neurobiology of virtual reality pain attenuation. Cyberpsychol Behav. 2007 Aug;10(4):536-44. doi: 10.1089/cpb.2007.9993. PMID: 17711362.
- Tack C. Virtual reality and chronic low back pain. Disabil Rehabil Assist Technol. 2021 Aug;16(6):637-645. doi: 10.1080/17483107.2019.1688399. Epub 2019 Nov 20. PMID: 31746250.
- Yalfani A, Abedi M, Raeisi Z. Effects of an 8-Week Virtual Reality Training Program on Pain, Fall Risk, and Quality of Life in Elderly Women with Chronic Low Back Pain: Double-Blind Randomized Clinical Trial. Games Health J. 2022 Apr;11(2):85-92. doi: 10.1089/g4h.2021.0175. Epub 2022 Mar 15. Erratum in: Games Health J. 2022 Aug;11(4):275. PMID: 35290742.
- Schulz KF, Altman DG, Moher D. CONSORT 2010 statement: Updated guidelines for reporting parallel group randomised trials. J Pharmacol Pharmacother. 2010 Jul;1(2):100-7. doi: 10.4103/0976-500X.72352. PMID: 21350618; PMCID: PMC3043330.
- Hien HA, Tam NM, Tam V, Derese A, Devroey D. Prevalence, Awareness, Treatment, and Control of Hypertension and Its Risk Factors in (Central) Vietnam. Int J Hypertens. 2018 May 16;2018:6326984. doi: 10.1155/2018/6326984. PMID: 29887994; PMCID: PMC5977008.
- Palsson TS, Hirata RP, Graven-Nielsen T. Experimental Pelvic Pain Impairs the Performance During the Active Straight Leg Raise Test and Causes Excessive Muscle Stabilization. Clin J Pain. 2015 Jul;31(7):642-51. doi: 10.1097/AJP.0000000000000139. PMID: 25119510.
- Chou R, Qaseem A, Snow V, Casey D, Cross JT Jr, Shekelle P, Owens DK; Clinical Efficacy Assessment Subcommittee of the American College of Physicians; American College of Physicians; American Pain Society Low Back Pain Guidelines Panel. Diagnosis and treatment of low back pain: a joint clinical practice guideline from the American College of Physicians and the American Pain Society. Ann Intern Med. 2007 Oct 2;147(7):478-91. doi: 10.7326/0003-4819-147-7-200710020-00006. Erratum in: Ann Intern Med. 2008 Feb 5;148(3):247-8. PMID: 17909209.
- Goodyear MD, Krleza-Jeric K, Lemmens T. The Declaration of Helsinki. BMJ. 2007 Sep 29;335(7621):624-5. doi: 10.1136/bmj.39339.610000.BE. PMID: 17901471; PMCID: PMC1995496.
- Mohammadi Nia Samakosh H, Brito JP, Shojaedin SS, Hadadnezhad M, Oliveira R. What Does Provide Better Effects on Balance, Strength, and Lower Extremity Muscle Function in Professional Male Soccer Players with Chronic Ankle Instability? Hopping or a Balance Plus Strength Intervention? A Randomized Control Study. Healthcare (Basel). 2022 Sep 21;10(10):1822. doi: 10.3390/healthcare10101822. PMID: 36292269; PMCID: PMC9602092.
- Borg GA. Psychophysical bases of perceived exertion. Med Sci Sports Exerc. 1982;14(5):377-81. PMID: 7154893..
- Garcia LM, Birckhead BJ, Krishnamurthy P, Sackman J, Mackey IG, Louis RG, Salmasi V, Maddox T, Darnall BD. An 8-Week Self-Administered At-Home Behavioral Skills-Based Virtual Reality Program for Chronic Low Back Pain: Double-Blind, Randomized, Placebo-Controlled Trial Conducted During COVID-19. J Med Internet Res. 2021 Feb 22;23(2):e26292. doi: 10.2196/26292. PMID: 33484240; PMCID: PMC7939946.
- Park JH. Effects of virtual reality-based spatial cognitive training on hippocampal function of older adults with mild cognitive impairment. Int Psychogeriatr. 2022 Feb;34(2):157-163. doi: 10.1017/S1041610220001131. Epub 2020 Jul 3. PMID: 32616109.
- Malfliet A, Kregel J, Coppieters I, De Pauw R, Meeus M, Roussel N, Cagnie B, Danneels L, Nijs J. Effect of Pain Neuroscience Education Combined With Cognition-Targeted Motor Control Training on Chronic Spinal Pain: A Randomized Clinical Trial. JAMA Neurol. 2018 Jul 1;75(7):808-817. doi: 10.1001/jamaneurol.2018.0492. Erratum in: JAMA Neurol. 2019 Mar 1;76(3):373. PMID: 29710099; PMCID: PMC6145763.
- Dolphens M, Nijs J, Cagnie B, Meeus M, Roussel N, Kregel J, Malfliet A, Vanderstraeten G, Danneels L. Efficacy of a modern neuroscience approach versus usual care evidence-based physiotherapy on pain, disability and brain characteristics in chronic spinal pain patients: protocol of a randomized clinical trial. BMC Musculoskelet Disord. 2014 May 8;15:149. doi: 10.1186/1471-2474-15-149. PMID: 24885889; PMCID: PMC4028010.
- Alfonsin MM, Chapon R, de Souza CAB, Genro VK, Mattia MMC, Cunha-Filho JS. Correlations among algometry, the visual analogue scale, and the numeric rating scale to assess chronic pelvic pain in women. Eur J Obstet Gynecol Reprod Biol X. 2019 May 2;3:100037. doi: 10.1016/j.eurox.2019.100037. PMID: 31403125; PMCID: PMC6687371.
- Jones T, Miller R, Street JT, Sawatzky B. Validation of the Oswestry Disability Index for pain and disability in arthrogryposis multiplex congenita. Ann Phys Rehabil Med. 2019 Mar;62(2):92-97. doi: 10.1016/j.rehab.2018.05.1319. Epub 2018 Jun 9. PMID: 29894799.
- Mokhtarinia HR, Hosseini A, Maleki-Ghahfarokhi A, Gabel CP, Zohrabi M. Cross-cultural adaptation, validity, and reliability of the Persian version of the spine functional index. Health Qual Life Outcomes. 2018 May 15;16(1):95. doi: 10.1186/s12955-018-0928-5. PMID: 29764442; PMCID: PMC5952597.
- Perron M, Gendron C, Langevin P, Leblond J, Roos M, Roy JS. Prognostic factors of a favorable outcome following a supervised exercise program for soldiers with sub-acute and chronic low back pain. BMC Musculoskelet Disord. 2018 Apr 2;19(1):95. doi: 10.1186/s12891-018-2022-x. PMID: 29606114; PMCID: PMC5879551.
- Nedjat S, Montazeri A, Holakouie K, Mohammad K, Majdzadeh R. Psychometric properties of the Iranian interview-administered version of the World Health Organization's Quality of Life Questionnaire (WHOQOL-BREF): a population-based study. BMC Health Serv Res. 2008 Mar 21;8:61. doi: 10.1186/1472-6963-8-61. PMID: 18366715; PMCID: PMC2287168.
- Khatua DK. Psychological comorbidity of chronic low back pain. IJPMR. 2011; 22: 7-11.
- García-Rodríguez LC, Carreño-Moreno S, Chaparro-Díaz L. Instrumentos para la medición de sobrecarga del cuidador en pacientes con enfermedad crónica: revisión psicométrica. Salud UIS. 2023; 55.
- Nejat S. The World Health Organization Quality of Life (WHOQOL-BREF) questionnaire: Translation and validation study of the Iranian version. Journal of school of public health and institute of public health research. 2006; 4(4): 1-12.
- Klaassen RJ, Barrowman N, Merelles-Pulcini M, Vichinsky EP, Sweeters N, Kirby-Allen M, Neufeld EJ, Kwiatkowski JL, Wu J, Vickars L, Blanchette VS, Forgie M, Yamashita R, Wong-Rieger D, Young NL. Validation and reliability of a disease-specific quality of life measure (the TranQol) in adults and children with thalassaemia major. Br J Haematol. 2014 Feb;164(3):431-7. doi: 10.1111/bjh.12631. Epub 2013 Nov 3. PMID: 24180641.
- Keselman HJ. Statistical practices of educational researchers: An analysis of their ANOVA, MANOVA, and ANCOVA analyses. Review of educational research. 1998; 68(3): 350-386.
- Faul F, Erdfelder E, Lang AG, Buchner A. G*Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods. 2007 May;39(2):175-91. doi: 10.3758/bf03193146. PMID: 17695343.
- Mbada CE. Comparative effects of clinic-and virtual reality-based McKenzie extension therapy in chronic non-specific low-back pain. Human Movement. 2019; 20(3): 66-79.
- Alemanno F, Houdayer E, Emedoli D, Locatelli M, Mortini P, Mandelli C, Raggi A, Iannaccone S. Efficacy of virtual reality to reduce chronic low back pain: Proof-of-concept of a non-pharmacological approach on pain, quality of life, neuropsychological and functional outcome. PLoS One. 2019 May 23;14(5):e0216858. doi: 10.1371/journal.pone.0216858. PMID: 31120892; PMCID: PMC6532874.
- Wood L, Hendrick PA. A systematic review and meta-analysis of pain neuroscience education for chronic low back pain: Short-and long-term outcomes of pain and disability. Eur J Pain. 2019 Feb;23(2):234-249. doi: 10.1002/ejp.1314. Epub 2018 Oct 14. PMID: 30178503.
- Solouki S, Pooyan M. Arrangement and Applying of Movement Patterns in the Cerebellum Based on Semi-supervised Learning. Cerebellum. 2016 Jun;15(3):299-305. doi: 10.1007/s12311-015-0695-3. PMID: 26109488.
- Saragiotto BT, Maher CG, Yamato TP, Costa LOP, Costa LCM, Ostelo RWJG, Macedo LG. Motor Control Exercise for Nonspecific Low Back Pain: A Cochrane Review. Spine (Phila Pa 1976). 2016 Aug 15;41(16):1284-1295. doi: 10.1097/BRS.0000000000001645. PMID: 27128390.
- Hodges P, van den Hoorn W, Dawson A, Cholewicki J. Changes in the mechanical properties of the trunk in low back pain may be associated with recurrence. J Biomech. 2009 Jan 5;42(1):61-6. doi: 10.1016/j.jbiomech.2008.10.001. Epub 2008 Dec 4. PMID: 19062020.
- Macedo LG, Latimer J, Maher CG, Hodges PW, McAuley JH, Nicholas MK, Tonkin L, Stanton CJ, Stanton TR, Stafford R. Effect of motor control exercises versus graded activity in patients with chronic nonspecific low back pain: a randomized controlled trial. Phys Ther. 2012 Mar;92(3):363-77. doi: 10.2522/ptj.20110290. Epub 2011 Dec 1. Erratum in: Phys Ther. 2012 Apr;92(4):631. PMID: 22135712.
- Thiamwong L, Stout JR, Sole ML, Ng BP, Yan X, Talbert S. Physio-Feedback and Exercise Program (PEER) Improves Balance, Muscle Strength, and Fall Risk in Older Adults. Res Gerontol Nurs. 2020 Nov 1;13(6):289-296. doi: 10.3928/19404921-20200324-01. Epub 2020 Apr 14. PMID: 32286669.
- Cohen JP, Mendoza M, Roland C. Challenges Involved in the Development and Delivery of Abuse-deterrent Formulations of Opioid Analgesics. Clin Ther. 2018 Feb;40(2):334-344. doi: 10.1016/j.clinthera.2018.01.003. Epub 2018 Feb 3. PMID: 29398162.
Article Alerts
Subscribe to our articles alerts and stay tuned.
 This work is licensed under a Creative Commons Attribution 4.0 International License.
This work is licensed under a Creative Commons Attribution 4.0 International License.

 Save to Mendeley
Save to Mendeley
