Journal of Novel Physiotherapy and Physical Rehabilitation
Assessment Batteries Used in Pediatric Rehabilitation
Fuat Sonmez1, Deniz Cakir2, Emre Demir3 and Nilay Comuk Balci2*
1Professor, Dr. Ilhan Ozdemir Training and Research Hospital, Giresun, Turkey
2Department of Physiotherapy and Rehabilitation, Ondokuz Mayis University, Faculty of Health Sciences, Samsun, Turkey
3Giresun Physical Medicine and Rehabilitation Center, Giresun, Turkey
Cite this as
Sonmez F, Cakir D, Demir E, Balci NC. Assessment Batteries Used in Pediatric Rehabilitation. J Nov Physiother Phys Rehabil. 2024;11(2):022-033. DOI: 10.17352/2455-5487.000106Copyright
© 2024 Sonmez F, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.Background: Classifying tools used for the pediatric population can expedite the creation of preventive, diagnostic, and therapeutic strategies, helping to identify factors influencing this group and enhancing their development.
Objectives: This study aims to present the assessment batteries used in the pediatric population together so that assessors and practitioners can easily examine the batteries and decide which test battery to use.
Method: Seventy questionnaire scales used in pediatric rehabilitation were compiled from the electronic database.
Results: There are many batteries used in the pediatric population. Categorizing these batteries provides significant advantages and convenience for readers.
Conclusion: In pediatric rehabilitation, various assessment batteries are used to assess the abilities and development of children, and these tools vary according to age groups. Different tools have been determined in areas such as motor, sensory, neuromuscular, cognitive, and family assessments, and each significantly impacts children’s development. By defining reliable assessment methods for each area, it is aimed to develop early intervention and appropriate treatment strategies.
Introduction
Children develop at different rates, and it is important to distinguish those within the “normal” range from those following a pathological course [1]. There is good evidence that early identification and early intervention improve the outcomes of children with developmental impairments [2,3]. During fetal life and the first two years postnatally, the brain shows strong developmental activity. High developmental activity implies high neuroplasticity, suggesting that especially the first year offers great opportunities for early intervention to improve the child’s developmental outcome [4]. Given the importance of the early years, early intervention is crucial. Because learning is cumulative, barriers to healthy development early in life impede development at each subsequent stage [5]. Interventions can include physiotherapy, occupational therapy, psychology, neurodevelopmental treatment, parent-infant relationship enhancement, infant stimulation, infant development, developmental care, and education [6]. These interventions aim to prevent or minimize motor, cognitive, and emotional disorders in young children who are disadvantaged due to biological or environmental risk factors. In this context, the environment, social relationships, and parents have an important role in early intervention [6]. Namely, interventions that are tailored to the family, the child, and their interaction, may be successful [4].
Illnesses, injuries, and different disease processes can have a profound impact on the attainment of developmental milestones, with delays noted in gross motor, fine motor, speech and language, and/or psychosocial areas [7]. Genetic factors may also determine the fundamental developmental potential, but environmental factors also have crucial influences on the profile achieved. Positive experiences during early childhood may enhance brain development, particularly in the area of linguistic and social skills [1]. Environmental factors are a fundamental determinant of early child development and, in turn, early child development is a determinant of health, well-being, and learning skills across the balance of the life course [8]. Environmental factors play a critical role in the early phases of conception, pregnancy, and post-natal periods of child development. Sensitive periods in brain and biological development start prenatally and continue throughout childhood and adolescence. The extent to which these processes lead to healthy development depends upon the qualities of stimulation, support, and nurturance in the social environments in which children live, learn, and grow [9].
Considering that very rapid progress is seen in all developmental areas in early childhood, it is very important to support, evaluate, and monitor each developmental area correctly during this period. These developmental areas are; cognitive, language, social-emotional, motor, and self-care, which is not a developmental area but includes skills that are important for the child in this period. Since all these developmental areas should be developed in a balanced way, one developmental area should not be held back from the other and each should be supported equally [10].
A thorough understanding of the developmental milestones and the age at which the child attained them can assist with diagnosis and treatment protocols. Many tools can be used to evaluate and quantify functional status, developmental skills, cognition and potential for academic achievement, visual motor abilities, a child’s social and adaptive skills, and perceived quality of life, disability, and perception, in the pediatric population [7]. Measurement tools are standardized instruments evaluated for their psychometric properties and used to measure the change in a person’s health status through quantitative assessment of function [11]. These tools are effective for use in the clinical setting because standardized outcome measures provide a common language among physical therapists [12]. The choice of an assessment tool is determined by the purpose of assessing [13].
During pediatric rehabilitation practices, children’s competencies in different areas and their abilities should be assessed at different times to create a program and determine its effectiveness [14]. There is a wide variety of tools available in the field of pediatric rehabilitation to help determine appropriate treatment and its effectiveness and to identify the child’s strengths and weaknesses in all areas [7,15]. For these assessments to be standardized and meaningful, different researchers have developed various assessment tools, and both the reliability and validity of these tools have been investigated and translated into different languages [14].
This study aims to investigate the effectiveness and standardization of assessment tools used in different areas of pediatric rehabilitation practice by examining the current evidence that early intervention improves the outcomes of children with developmental disorders and emphasizing the importance of accurate assessment and support of children’s developmental processes in the early period.
Method
We have searched in the PubMed, MEDLINE (Ovid), EMBASE (Ovid), Cochrane, CINAHL (EBSCO), WILEY, Web of Science, PEDro, and Scopus databases with the keywords of:
- Motor Assessment Batteries in Childhood
- Sensory Assessment Batteries in Childhood
- Cognitive Assessment Batteries in Childhood
- Family Assessment Batteries in Childhood
- Life Quality Assessment Batteries in Childhood
- Visual Assessment Batteries in Childhood
- Neuro-muscular Assessment Batteries in Childhood
- Brachial Pleksus (BP) Assessment Batteries in Childhood
- Neuro-motor Assessment Batteries in Childhood
- Multi-Dimensional Assessment Batteries in Childhood
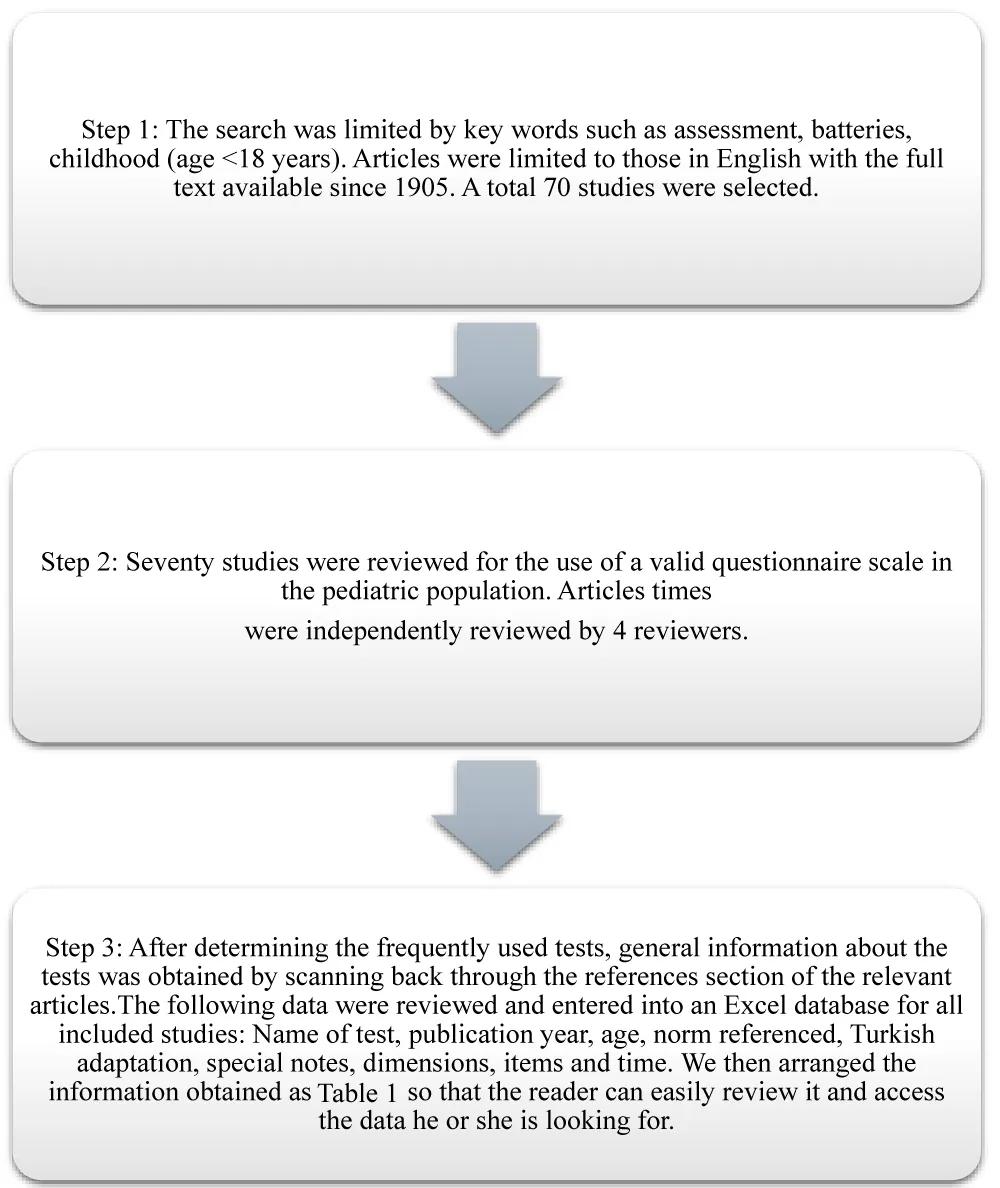
A comprehensive search of the database was conducted in August 2024, for studies concerning the Assessment Batteries in childhood by using the following steps (Figure 1), Table 1:
Results
Characteristics of the included studies
The characteristics of the included studies were assessed in several dimensions: Name of the test, publication year, age, norm-referenced, Turkish adaptation, special notes, dimensions, items, and time.
Batteries used to assess the pediatric population
To evaluate batteries used in the pediatric population, 70 different tools were identified and divided into 10 categories: Motor Assessment Batteries, Sensory Assessment Batteries, Cognitive Assessment Batteries, Family Assessment Batteries, Quality of Life Assessment Batteries, Visual Assessment Batteries, Neuro-muscular Assessment Batteries, Brachial Plexus (BP) Assessment Batteries, Multi-Dimensinal Assessment Batteries, Neuro-motor Assessment Batteries.
Physiotherapists use motor assessment batteries in pediatric rehabilitation to determine children’s motor abilities and disabilities with motor development [16]. Motor development is a result of changes in time [17] so we need different assessment tools for the ages. For this purpose, we determined motor assessment tools for different age groups. Some of the assessment batteries are focused on very specific time window such as Test of Infant Motor Profile (TIMP) [18], Harris Infant Neuromotor Test (HINT) [19], Alberta Infant Motor Scale (AIMS) [20], Movement Assessment of Infants (MAI) [21], Infant Motor Profile (IMP) [22], Movement Assessment of Children (MAC) [23], Milani-Comporetti Developmental Examination [24] and some tools have wider time Windows such as Bruininks-Oseretsky Test of Motor Proficiency, Second Edition (BOT-2) [25] and Movement Assessment Battery for Children (Movement ABC-2) [26].
We perceive our environment with our senses, and children’s perception of the environment is different from adults due to their developmental stage [27]. Assessing the senses of children we identified six different assessment tools. The Nottingham Sensory Assessment tool doesn’t have any age limitation because it assesses senses in general [28]. Some tools assess more specific senses for age groups such as the Sensory Integration and Praxis Test (SIPT) [29], The Test of Sensory Function in Infants [30], The Sensory Rating Scale [31], Sensory Processing Measure, Sensory Processing Measure Pre-School [32].
Cognitive assessment is used mainly when a child shows clues of developmental delay or suspects of delay. Although there are norm-referenced cognitive assessment tools some scholars raised concerns about tools adequacies [33]. Therefore we tried to determine tools with different abilities. There are well-established and almost traditional tools like The Stanford-Binet Intelligence Scale [34], Wechsler Intelligence Scale for Children (WISC-R) [35], Cattell Intelligence Test [36], Cognitive Assessment System(CAS) [37], Children’s Apperception Test (CAT) [38], Leiter international performance scale-revised (Leiter-R) [39], some newer tools that developed more recently and less time consuming like Behavior Rating Inventory of Executive Function (BRIEF) [40] some developed specifically a culture’s people like Anatolian-Sak Intelligence Scale: The First Turkish Intelligence Test [41] and some of the tools are technologically enhanced like MOXO d-CPT [42].
Family is our first social environment and has a great impact on children’s development [43] so we need to evaluate family as well. For this purpose we identified The McMaster family assessment device [44], Family Participation Scale [45], The Family Adaptability and Cohesion Evaluation Scale (FACES IV) [46], Caregiver Difficulties Scale (CDS) [47], Family Strengths Inventory [48] as internationally used and cross-referenced tools and “The Perceived Family Functioning Scale (PFFS),” a tool that specifically developed for Turkish culture [49].
Various assessment batteries are used for the classification and evaluation of brachial plexus injuries [50]. Narakas is the method used for motor and sensory classification in the brachial plexus [51]. Batteries such as Quality of Upper Extremity Skills Test (QUEST) [52], Melbourne Assessment 2 (MA-2) [53], The Active Movement Scale (AMS) [54], Functional Dexterity Test (FDT) [55], Assisting Hand Assessment (AHA) [56], The Children Hand Use Experience (CHEQ) [57], Brachial Pleksus Outcome Measure (BPOM) [58], Pediatric Motor Activity Log-Revised (PMAL-R) [59] are used to evaluate the quality of movement and motor skills. ABILHAND-Kids [60] and Disability of the Arm, Shoulder, and Hand (DASH) [61] evaluate daily life activities.
World Health Organization (WHO) defines health as a state of complete physical, mental, and social well-being, not the absence of disease or infirmity, in 1948 [62]. And quality of life assessment batteries have become more important in general health assessment. The Assessment of Life Habits (LIFE-H) [63], Pediatric Evaluation of Disability Inventory (PEDI) [64], Pediatric Outcome Data Collection Instrument (PODCI) [65], Pediatric Quality of Life Inventory [66], Child Health Questionnaire (CHQ) [67] are effective batteries that evaluate the quality of life in multiple aspects.
Visual skills directly affect motor and sensory functions at every stage of a person’s life. For this reason, assessment of visual functions is one of the important points in developing motor and sensory skills. Batteries such as Motor-Free Visual Perception Test-3 [68], Central Visual Impairment (CVI) Questionnaire [69], Visual Skills İnventory [70] and Frostig Developmental Test of Visual Perception [71] can evaluate visual skills precisely and effectively.
Neuromuscular disorders are a diverse group of problems that affect how muscles and neurons work. Motor neurons, nerves, neuromuscular junctions, and muscles can be affected by these problems depending on the specific disorder. The results of these disorders can be very severe, even lethal. Thus proper evaluation and re-evaluation are crucial in this disorder [72]. We determined Hammersmith Motor Ability Score [73], The North Star Ambulatory Assessment [74], Brooke Upper Extremity Functional Rating Scale [75], Vignos Functional Rating Scale [76], The Motor Function Measure (MFM) [77], The Egen Klassifikation (EK) Scale [78], The quick motor function test (QMFT) [79], The Children’s Hospital of Philadelphia Infant Test of Neuromuscular Disorders (CHOP INTEND) [80], Upper Limb Short Questionnaire [81] are reliable tools for evaluating children with neuromuscular disorders.
Hammersmith Neonatal Neurological Examination (HNNE) [82], and Standardized Infant NeuroDevelopmental Assessment (SINDA) [83] are some of the tools used for neuromotor assessment. General Movement Assessment (GMA) [84] and Hammersmith Infant Neurological Examination (HINE) [85] are the two neuromotor assessment tools that have great value for cerebral palsy risk detection [86]. With the support of magnetic resonance imaging, these two tools have the highest evidence rate for accurately determining children with cerebral palsy [87]. The Neonatal Infant Motor Assessment Scale (NIMAS) however is one of the most recent tools for neuromotor assessment [88].
There are some limitations in our study. The first of these is that our search was not systematic, and the other is that only some database (PubMed, MEDLINE (Ovid), EMBASE (Ovid), WILEY, Web of Science, PEDro, and Scopus) was scanned. In future studies, systematic research covering multiple databases would be beneficial.
Conclusion
The assessment of the pediatric population is of great importance. These assessments should take a holistic approach to the child. There are many assessment batteries used in pediatrics and many of the batteries used have been tested for reliability and validity with adequate features. Before deciding on a tool to be used, the content of the elements of the tool should be examined thoroughly. Categorizing these tools can accelerate the development of preventive, diagnostic, and therapeutic strategies to determine the factors affecting the pediatric population and to support and improve the development of this population in pediatric rehabilitation clinics.
- Bellman M, Byrne O, Sege R. Developmental assessment of children. BMJ. 2013;346(7891):e8687. Available from: https://doi.org/10.1136/bmj.e8687
- Gomby DS, Larner MB, Stevenson CS, Lewit EM, Behrman RE. Long-term outcomes of early childhood programs: analysis and recommendations. The Future of Children / Center for the Future of Children, the David and Lucile Packard Foundation. 1995;5(3):6-24. Available from: https://pubmed.ncbi.nlm.nih.gov/8835513/
- Guralnick MJ. The effectiveness of early intervention. Paul H. Brookes Publishing Co.; 1997; 665. Available from: https://eric.ed.gov/?id=ED414694
- Hadders-Algra M. Early diagnostics and early intervention in neurodevelopmental disorders—age-dependent challenges and opportunities. J Clin Med. 2021;10(4):861. Available from: https://doi.org/10.3390/jcm10040861
- Cioni G, Inguaggiato E, Sgandurra G. Early intervention in neurodevelopmental disorders: underlying neural mechanisms. Dev Med Child Neurol. 2016;58 Suppl 4:61–66. Available from: https://doi.org/10.1111/dmcn.13050
- Guralnick MJ. Why early intervention works: a systems perspective. Infants Young Child. 2011;24(1):6–28. Available from: https://doi.org/10.1097/iyc.0b013e3182002cfe
- Cifu DX. Braddom’s physical medicine and rehabilitation. 6th ed. Elsevier; 2020;52.
- Maggi S, Irwin LJ, Siddiqi A, Hertzman C. The social determinants of early child development: an overview. J Paediatr Child Health. 2010;46(11):627–635. Available from: https://doi.org/10.1111/j.1440-1754.2010.01817.x
- World Health Organization. The importance of caregiver-child interactions for the survival and healthy development of young children: a review. 2004. Available from: https://www.who.int/publications/i/item/924159134X
- Kılıç Z, Balat GU, Sarı SÇ. Adaptation study of CHAMPS motor skills protocol (CMSP) into Turkish for 4 and 5 year old children. Journal of Educational Theory and Practice Research. 2017;3:129–42. Available from: https://dergipark.org.tr/tr/download/article-file/367044
- Jette DU, Halbert J, Iverson C, Miceli E, Shah P. Use of standardized outcome measures in physical therapist practice: perceptions and applications. Phys Ther. 2009;89(2):125-135. Available from: https://doi.org/10.2522/ptj.20080234
- American Physical Therapy Association. Outcomes measurement. 2020. Available from: https://www.apta.org/your-practice/outcomes-measurement
- Chawarska K, Klin A, Volkmar FR. Autism spectrum disorders in infants and toddlers. 2008;116.
- 1Sonksen M. Developmental assessment. In: Yazıcı M, Kerem G. M, editors. Hippocrates Publishing; 2019;370.
- Erkin G, Elhan AH, Aybay C, Sirzai H, Ozel S. Validity and reliability of the Turkish translation of the Pediatric Evaluation of Disability Inventory (PEDI). Disabil Rehabil. 2007;29(16):1271–1279. Available from: https://doi.org/10.1080/09638280600964307
- Tieman BL, Palisano RJ, Sutlive AC. Assessment of motor development and function in preschool children. Ment Retard Dev Disabil Res Rev. 2005;11(3):189-196. Available from: https://doi.org/10.1002/mrdd.20074
- Clark JE, Whitall J. What is motor development? The lessons of history. Quest. 1989;41(3):183-202. Available from: https://doi.org/10.1080/00336297.1989.10483969
- Campbell SK, Osten ET, Kolobe THA, Fisher AG. Development of the Test of Infant Motor Performance. Phys Med Rehabil Clin N Am. 1993;4(3):541-550. Available from: https://doi.org/10.1093/ptj/75.7.585
- Harris SR, Megens AM, Backman CL, Hayes V. Development and standardization of the Harris Infant Neuromotor Test. Infants Young Child. 2003;16(2):143–51. Available from: http://dx.doi.org/10.1097/00001163-200304000-00006
- Darrah J, Piper M, Watt MJ. Assessment of gross motor skills of at-risk infants: predictive validity of the Alberta Infant Motor Scale. Dev Med Child Neurol. 1998;40(7):485-491. Available from: https://doi.org/10.1111/j.1469-8749.1998.tb15399.x
- Harris SR, Haley SM, Tada WL, Swanson MW. Reliability of observational measures of the Movement Assessment of Infants. Phys Ther. 1984;64(4):471-475. Available from: https://doi.org/10.1093/ptj/64.4.471
- Heineman KR, Bos AF, Hadders-Algra M. The Infant Motor Profile: a standardized and qualitative method to assess motor behavior in infancy. Dev Med Child Neurol. 2008;50(4):275-282. Available from: https://doi.org/10.1111/j.1469-8749.2008.02035.x
- Chandler LS, Terhorst L, Rogers JC, Holm MB. Movement Assessment of Children (MAC): validity, reliability, stability, and sensitivity to change in typically developing children. Child Care Health Dev. 2016;42(4):513–20. Available from: https://doi.org/10.1111/cch.12348
- Milani‐Comparetti A, Gidoni EA. Routine developmental examination in normal and retarded children. Dev Med Child Neurol. 1967;9(5):631-638. Available from: https://doi.org/10.1111/j.1469-8749.1967.tb02335.x
- Deitz JC, Kartin D, Kopp K. Review of the Bruininks-Oseretsky Test of Motor Proficiency, Second Edition (BOT-2). Phys Occup Ther Pediatr. 2007;27(4):87-102. Available from: https://pubmed.ncbi.nlm.nih.gov/18032151/
- Wagner MO, Kastner J, Petermann F, Bös K. Factorial validity of the Movement Assessment Battery for Children-2 (age band 2). Res Dev Disabil. 2011;32(2):674-680. Available from: https://doi.org/10.1016/j.ridd.2010.11.016
- Turgay ZT, Sarıberberoğlu MT. The role of the senses in children’s perception of space. ICONARP Int J Archit Plann. 2022;10(1):70–96. Available from: http://dx.doi.org/10.15320/ICONARP.2022.194
- Lincoln NB, Jackson JM, Adams SA. Reliability and revision of the Nottingham Sensory Assessment for stroke patients. Physiotherapy. 1998;8(84):358-365. Available from: http://dx.doi.org/10.1016%2FS0031-9406(05)61454-X
- Ayres A. Sensory integration and praxis tests (SIPT). 1996. Available from: https://paa.com.au/wp-content/uploads/2018/12/SIPT-Sample-Test-Report.pdf
- Jirikowic TL, Engel JM, Deitz JC. The Test of Sensory Functions in Infants: test-retest reliability for infants with developmental delays. Am J Occup Ther. 1997;51(9):733-738. Available from: https://doi.org/10.5014/ajot.51.9.733
- Provost B, Oetter P. The Sensory Rating Scale for infants and young children. Phys Occup Ther Pediatr. 1994;13(4):15-35. Available from: http://dx.doi.org/10.1080/J006v13n04_02
- Jorquera-Cabrera S, Romero-Ayuso D, Rodriguez-Gil G, Triviño-Juárez JM. Assessment of sensory processing characteristics in children between 3 and 11 years old: a systematic review. Front Pediatr. 2017;5:57. Available from: https://doi.org/10.3389/fped.2017.00057
- Bradley-Johnson S. Cognitive assessment for the youngest children: a critical review of tests. 2001;19(1):19-44. Available from: http://dx.doi.org/10.1177/073428290101900102
- Roid G, Pomplun M. The Stanford-Binet Intelligence Scales, fifth edition. 2012;249-268. Available from: https://psycnet.apa.org/record/2012-09043-010
- Savaşir I, Şahin N. Wechsler intelligence scale for children. 1995. Available from: https://toad.halileksi.net/olcek/wechsler-cocuklar-icin-zeka-olcegi/
- Horn JL, Cattell RB. Refinement and test of the theory of fluid and crystallized general intelligences. J Educ Psychol. 1966;57(5):253-270. Available from: https://doi.org/10.1037/h0023816
- Naglieri JA, Otero TM. The assessment of executive function using the Cognitive Assessment System: second edition. In: Handbook of Executive Functioning. 2014;191–208.
- Byrd E, Witherspoon RL. Responses of preschool children to the Children’s Apperception Test. 1954;35-44. Available from: https://pubmed.ncbi.nlm.nih.gov/13199842/
- Roid GH, Miller LJ. Leiter International Performance Scale-Revised. Psychol Sch. 1997;10. Available from: https://www.scirp.org/reference/referencespapers?referenceid=1268679
- Gioia GA, Isquith PK, Guy SC, Kenworthy L, Baron IS. Behavior rating inventory of executive function. Child Neuropsychol. 2000;6(3):235-238. Available from: https://doi.org/10.1076/chin.6.3.235.3152
- Kalaycı N, Aydınlı B. The evaluation of executed giftedness test in Turkey. Soc Sci Cent Issues. 2019;1(1):2-7. Available from: https://dergipark.org.tr/en/pub/ssci/issue/46453/573509
- Eroglu M, Yaksi N, Gundogdu U, Demirkapi E, Degirmencioglu E. Effects of sport on symptoms of attention deficit hyperactivity disorder and performance loss caused by distractors: evaluation with MOXO d-CPT. Turk J Child Adolesc Ment Health. 2023;30(2):137-145. Available from: http://dx.doi.org/10.4274/tjcamh.galenos.2022.20591
- Bronfenbrenner U, Morris P. The ecology of developmental processes. In: Wiley; 1998;993–1028. Available from: https://psycnet.apa.org/record/2005-01926-019
- Epstein NB, Baldwin LM, Bishop DS. The McMaster family assessment device. J Marital Fam Ther. 1983;9(2):171-180. Available from: http://dx.doi.org/10.1111/j.1752-0606.1983.tb01497.x
- Kazdin AE, Holland L, Crowley M, Breton S. Barriers to treatment participation scale: evaluation and validation in the context of child outpatient treatment. J Child Psychol Psychiatry. 1997;38(8):1051-1062. Available from: https://doi.org/10.1111/j.1469-7610.1997.tb01621.x
- Franklin C, Streeter CL, Springer DW. Validity of the FACES IV family assessment measure. Res Soc Work Pract. 2001;11(5):576-596. Available from: http://dx.doi.org/10.1177/104973150101100503
- Wijesinghe CJ, Fonseka P, Hewage CG. The development and validation of an instrument to assess caregiver burden in cerebral palsy: Caregiver Difficulties Scale. Ceylon Med J. 2013;58(4):162-167. Available from: https://doi.org/10.4038/cmj.v58i4.5617
- Arshat Z, Baharudin R. Psychometric evaluation of the Australian inventory of family strengths (AIFS) on rural Malay families in Malaysia. Pertanika J Soc Sci Hum. 2014;22(1):271–84. Available from: https://www.researchgate.net/publication/289011142_Psychometric_evaluation_of_the_Australian_Inventory_of_Family_Strengths_AIFS_on_rural_Malay_families_in_Malaysia
- Özabacı N, Körük S. Development of the Perceived Family Functioning Scale (PADS): examination of its psychometric properties. Giant Perceived Family Functioning Scale (PFFS): Investigation of Its Psychometric Properties. 2021;4(2):53-72. Available from: https://dergipark.org.tr/tr/download/article-file/1934533
- Smania N, Berto G, La Marchina E, Melotti C, Midiri A, Roncari L, et al. Rehabilitation of brachial plexus injuries in adults and children. Eur J Phys Rehabil Med. 2012;48(3):483–506. Available from: https://pubmed.ncbi.nlm.nih.gov/23075907/
- Narakas AO, Hentz VR. Neurotization in brachial plexus injuries: indication and results. Clin Orthop Relat Res. 1988;(237):43-56. Available from: https://pubmed.ncbi.nlm.nih.gov/3056647/
- Dematteo C, Law M, Russell D, Pollock N, Rosenbaum P, Walter S. The reliability and validity of the quality of upper extremity skills test. Phys Occup Ther Pediatr. 1993;13(2):1-18. Available from: http://dx.doi.org/10.1080/J006v13n02_01
- Hoyt CR, Brown SK, Sherman SK, Wood-Smith M, Van AN, Ortega M, et al. Using accelerometry for measurement of motor behavior in children: relationship of real-world movement to standardized evaluation. Res Dev Disabil. 2020;96:103546. Available from: https://doi.org/10.1016/j.ridd.2019.103546
- Curtis C, Stephens D, Clarke HM, Andrews D. The active movement scale: an evaluative tool for infants with obstetrical brachial plexus palsy. J Hand Surg. 2002;27(3):470-478. Available from: https://doi.org/10.1053/jhsu.2002.32965
- Aaron DH, Stegink Jansen CW. Development of the Functional Dexterity Test (FDT): construction, validity, reliability, and normative data. J Hand Ther. 2003;16(1):12–21. Available from: https://doi.org/10.1016/s0894-1130(03)80019-4
- Krumlinde-Sundholm L, Holmefur M, Kottorp A, Eliasson AC. The Assisting Hand Assessment: current evidence of validity, reliability, and responsiveness to change. Dev Med Child Neurol. 2007;49(4):259-264. Available from: https://doi.org/10.1111/j.1469-8749.2007.00259.x
- Sköld A, Hermansson LN, Krumlinde-Sundholm L, Eliasson AC. Development and evidence of validity for the Children’s Hand-use Experience Questionnaire (CHEQ). Dev Med Child Neurol. 2011;53(5):436-442. Available from: https://doi.org/10.1111/j.1469-8749.2010.03896.x
- Ho ES, Curtis CG, Clarke HM. The brachial plexus outcome measure: development, internal consistency, and construct validity. J Hand Ther. 2012;25(4):406–17. Available from: https://doi.org/10.1016/j.jht.2012.05.002
- Uswatte G, Taub E, Griffin A, Vogtle L, Rowe J, Barman J. The Pediatric Motor Activity Log-Revised: assessing real-world arm use in children with cerebral palsy. Rehabil Psychol. 2012;57(2):149-158. Available from: https://doi.org/10.1037/a0028516
- Arnould C, Penta M, Renders A, Thonnard JL. ABILHAND-Kids: a measure of manual ability in children with cerebral palsy. Neurology. 2004;63(6):1045-1052. Available from: https://doi.org/10.1212/01.wnl.0000138423.77640.3761 .
- Jester A, Harth A, Wind G, Germann G, Sauerbier M. Disabilities of the arm, shoulder, and hand (DASH) questionnaire: determining functional activity profiles in patients with upper extremity disorders. J Hand Surg Br. 2005;30(1):23-28. Available from: https://doi.org/10.1016/j.jhsb.2004.08.008
- WHO. Constitution of the World Health Organization. 2006. Available from: https://www.afro.who.int/sites/default/files/pdf/generic/who_constitution_en.pdf
- Fougeyrollas P, Noreau L, Bergeron H, Cloutier R, Dion SA, St-Michel G. Social consequences of long-term impairments and disabilities: conceptual approach and assessment of handicap. Int J Rehabil Res. 1998;21(2):127–41. Available from: https://doi.org/10.1097/00004356-199806000-00002
- Berg M, Jahnsen R, Frøslie KF, Hussain A. Reliability of the Pediatric Evaluation of Disability Inventory (PEDI). Phys Occup Ther Pediatr. 2004;24(3):61-77. Available from: https://doi.org/10.1300/j006v24n03_05
- Lerman JA, Sullivan E, Barnes DA, Haynes RJ. The Pediatric Outcomes Data Collection Instrument (PODCI) and functional assessment of patients with unilateral upper extremity deficiencies. J Pediatr Orthop. 2005;25(3):405-407. Available from: https://doi.org/10.1097/01.bpo.0000149866.80894.70
- Varni JW, Limbers CA. The pediatric quality of life inventory: measuring pediatric health-related quality of life from the perspective of children and their parents. Pediatr Clin North Am. 2009;56(4):843-863. Available from: https://doi.org/10.1016/j.pcl.2009.05.016
- Landgraf JM. Child Health Questionnaire (CHQ). In: Encyclopedia of Quality of Life and Well-Being Research. 2021;1–6. Available from: http://dx.doi.org/10.1007/978-3-319-69909-7_324-2
- Colarusso RP, Hammill DD. Motor Free Visual Perceptual Test. Academic Therapy Publications; 1972.
- Ortibus E, Laenen A, Verhoeven J, De Cock P, Casteels I, Schoolmeesters B, et al. Screening for cerebral visual impairment: value of a CVI questionnaire. Neuropediatrics. 2011;42(4):138-147. Available from: https://doi.org/10.1055/s-0031-1285908
- McCulloch DL, Mackie RT, Dutton GN, Bradnam MS, Day RE, McDaid GJ, et al. A visual skills inventory for children with neurological impairments. Dev Med Child Neurol. 2007;49(10):757-763. Available from: https://doi.org/10.1111/j.1469-8749.2007.00757.x
- Corah NL, Powell BJ. A factor analytic study of the Frosting Developmental Test of Visual Perception. Percept Mot Skills. 1963;16:59–63. Available from: https://doi.org/10.2466/pms.1963.16.1.59
- Chikkannaiah M, Reyes I. New diagnostic and therapeutic modalities in neuromuscular disorders in children. Curr Probl Pediatr Adolesc Health Care. 2021;51(7):101033. Available from: https://doi.org/10.1016/j.cppeds.2021.101033
- Mercuri E, Messina S, Battini R, Berardinelli A, Boffi P, Bono R, et al. Reliability of the Hammersmith functional motor scale for spinal muscular atrophy in a multicentric study. Neuromuscul Disord. 2006;16(2):93-98. Available from: https://doi.org/10.1016/j.nmd.2005.11.010
- Mazzone ES, Messina S, Vasco G, Main M, Eagle M, D’Amico A, et al. Reliability of the North Star Ambulatory Assessment in a multicentric setting. Neuromuscul Disord. 2009;19(7):458-461. Available from: https://doi.org/10.1016/j.nmd.2009.06.368
- Davoli GBDQ, Cardoso J, Silva GC, Moreira R de FC, Mattiello-Sverzut AC. Instruments to assess upper-limb function in children and adolescents with neuromuscular diseases: a systematic review. Dev Med Child Neurol. 2021;63(9):1030-1037. Available from: https://doi.org/10.1111/dmcn.14887
- Vignos PJ, Spencer GE, Archibald KC. Management of progressive muscular dystrophy in childhood. JAMA. 1963;184(2):89–96. Available from: https://doi.org/10.1001/jama.1963.03700150043007
- De Lattre C, Payan C, Vuillerot C, Rippert P, De Castro D, Bérard C, et al. Motor function measure: validation of a short form for young children with neuromuscular diseases. Arch Phys Med Rehabil. 2013;94(11):2218-2226. Available from: https://doi.org/10.1016/j.apmr.2013.04.001
- Karaduman A, Tunca Ö. Turkish version of the Egen Klassifikation scale version 2: validity and reliability in the Turkish population. 2014;643–50. Available from: https://pubmed.ncbi.nlm.nih.gov/26388596/
- Van Capelle CI, Van Der Beek NAME, De Vries JM, Van Doorn PA, Duivenvoorden HJ, Leshner RT, et al. The quick motor function test: a new tool to rate clinical severity and motor function in Pompe patients. J Inherit Metab Dis. 2012;35(2):317–23. Available from: https://doi.org/10.1007/s10545-011-9388-3
- Glanzman AM, Mazzone E, Main M, Pelliccioni M, Wood J, Swoboda KJ, et al. The Children’s Hospital of Philadelphia Infant Test of Neuromuscular Disorders (CHOP INTEND): test development and reliability. Neuromuscul Disord. 2010;20(3):155-161. Available from: https://doi.org/10.1016/j.nmd.2009.11.01481.
- Janssen MMHP, Geurts ACH, de Groot IJM. Towards a short questionnaire for stepwise assessment of upper limb function, pain, and stiffness in Duchenne muscular dystrophy. Disabil Rehabil. 2018;40(7):842-847. Available from: https://doi.org/10.1080/09638288.2016.1274336
- Venkata SKRG, Pournami F, Prabhakar J, Nandakumar A, Jain N. Disability Prediction by Early Hammersmith Neonatal Neurological Examination: A Diagnostic Study. J Child Neurol. 2020;35(11):731-736. Available from: https://doi.org/10.1177/0883073820930487
- Hadders-Algra M, Tacke U, Pietz J, Philippi H. SINDA: Standardized Infant NeuroDevelopmental Assessment. 2022;200. Available from: https://www.mackeith.co.uk/book/sinda/
- Einspieler C, Bos AF, Libertus ME, Marschik PB. The General Movement Assessment Helps Us to Identify Preterm Infants at Risk for Cognitive Dysfunction. Front Psychol. 2016;7:406. Available from: https://doi.org/10.3389/fpsyg.2016.00406
- Hammersmith Infant Neurological Examination (HINE). 2023. Available from: https://www.mackeith.co.uk/wp-content/uploads/2024/01/Hammersmith-Infant-Neurological-Examination-HINE-Guidance-notes-update-20.12.2023-v2.pdf
- Sönmez F. 0-12 Multidimensional Neurodevelopmental Evaluation of Babies at High Risk of Cerebral Palsy Between the Ages of Months. 2022. Available from: http://hdl.handle.net/11655/26541
- Novak I, Morgan C, Adde L, Blackman J, Boyd RN, Brunstrom-Hernandez J, et al. Early, Accurate Diagnosis and Early Intervention in Cerebral Palsy: Advances in Diagnosis and Treatment. JAMA Pediatr. 2017;171(9):897–907. Available from: https://doi.org/10.1001/jamapediatrics.2017.1689
- Akin MA, Balci NC, Demirsoz M. Revolutionizing Neonatal Care: A Comprehensive Assessment of Neuromotor Development in At-Risk Infants Using the Novel Neonatal Infant Motor Assessment Scale (NIMAS) Test Battery. Children (Basel). 2024;11(4):445. Available from: https://doi.org/10.3390/children11040445
Article Alerts
Subscribe to our articles alerts and stay tuned.
 This work is licensed under a Creative Commons Attribution 4.0 International License.
This work is licensed under a Creative Commons Attribution 4.0 International License.

 Save to Mendeley
Save to Mendeley
