Journal of Novel Physiotherapy and Physical Rehabilitation
The Impact of Pelvic Floor Exercises on the Quality of Life of Women with Urinary Incontinence – Analysis of Pregnancy and the Postpartum Period
Zarawski Marcin1, Kołomańska Daria2, Maj Maria2, Panicz Daria2, Opławski Marcin1 and Mazur-Bialy Agnieszka Irena2*
2Faculty of Health Science, Jagiellonian University Medical College, Grzegorzecka 20, 31-531 Krakow, Poland
Cite this as
Zarawski M, Kołomańska D, Maj M, Panicz D, Opławski M, et al. (2017) The Impact of Pelvic Floor Exercises on the Quality of Life of Women with Urinary Incontinence – Analysis of Pregnancy and the Postpartum Period. J Nov Physiother Phys Rehabil 4(2): 035-041. DOI: 10.17352/2455-5487.000044Background: Urinary incontinence is a common symptom observed in modern times, which may affect 7–37% of women aged 20–39 and 9–39% after the age of 60. Pregnancy and natural delivery are important risk factors increasing the likelihood of incontinence.
The context and purpose of the study: In the current study we evaluated the impact of pelvic floor muscle training on the occurrence and intensity of urine leakage in women in three different periods: during pregnancy, until 6 weeks postpartum and up to 12 months after childbirth. In addition, we examined the contribution of pelvic floor exercise to changes in the quality of life of women with urinary incontinence.
Results: According to our research, urinary incontinence may affect up to 45% of women in the postpartum period, and although subsequently its incidence significantly drops, incontinence substantially reduced the quality of life of the study group. Nevertheless, regular pelvic floor training was observed to not only reduce the frequency and intensity of urinary incontinence in both pregnancy and the postpartum period, but also significantly improve the quality of life of the subjects. Therefore, this group should be included in a special program focusing on the prevention and physiotherapy of incontinence.
Conclusions: Our study shows the importance of educating the public about the role of prophylaxis in the prevention of urinary incontinence and confirms that pelvic floor training is an effective method of prophylaxis and therapy of urine leakage during pregnancy and the postpartum period.
Introduction
According to the terminology of the International Continence Society (ICS), urinary incontinence (UI) is defined as uncontrolled leakage of urine through the urethra. Because of its complex etiology, UI is not referred to as an independent disease entity, but as a symptom [1]. The World Health Organization (WHO) has classified UI as one of the ten major health problems of present times among women [2], with a significant group represented by women in the perinatal period (by ICS data, 15% to 30% puerperal women) [3,4]. In 2016, the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) estimated that UI occurs in 25–45% of women. The problem affects 7–37% of women aged 20–39 and 9–39% after the age of 60 [5].
Causes of UI can be divided into: dysfunction of the bladder or urethra, and neurological or gynecological causes. Gynecological components include: the weakening of pelvic floor muscles, atrophic vaginitis, gynecological and obstetrical operations and pelvic organ prolapse [6]. Existing evidence indicates that both natural delivery [7–10], as well as the pregnancy itself [11], have a prominent impact on the functioning of pelvic floor muscles and the occurrence of urinary incontinence. UI as a problem is 6.1 times more common in women after a vaginal delivery than in women after a cesarean section [12], but after a third cesarean section the risk of incontinence becomes similar (37.7–38.9%) [11]. this shows that pregnancy is also a big burden to pelvic floor muscles. Based on these studies, it can be concluded that pregnancy itself is a risk factor of UI, and not only the type of delivery. A Swedish questionnaire survey showed an increased incidence of urinary incontinence in women giving birth more than three times (16.4%) compared to women giving birth only once (10.6%) and to nulliparous individuals (5.5%) [9]. Furthermore, UI affects pregnant women 3.3 times more often than nulliparous women, and one year after first childbirth UI occurrence is still significantly higher (2.5 times more often) than in nulliparous women [13].
The development of UI in women starts with atrophy and damage to pelvic floor structures such as muscles and nerves [14]. For instance, limited cooperation between a midwife and the woman in labor, especially during the second stage of a natural delivery, can result in pelvic floor muscle injury due to increased intra-abdominal pressure. Natural delivery can cause laxity of pubourethral and external urethral ligaments. The weakening of these structures may be one of many reasons for UI [9].
The aim of this paper is to identify the impact of UI on quality of life during pregnancy and the postpartum period and to present an evaluation of pelvic floor muscle training regarding disease prevention and quality of life improvement.
Materials and Methods
Aerobic function: Data obtained for the 6 mwt showed good reliability (Figure 1); for V O2peak: test/retest correlation r=0. 90, p<0.001, ICC=0.85; for peak ventilation: r=0.88, p<0.001, ICC=0.83; for peak heart rate: r=0.86, p<0.001, ICC=0.82; and for distance walked: r=0.87; p=0.007, ICC=0.80.
Study population
The research was conducted in the years 2015–2016 on a group of 80 women recruited among obstetric department patients in Krakow. The eligibility criteria for this study were: first pregnancy, natural delivery (excluding delivery with forceps or vacuum extraction), and patient’s consent to participate in the research.
Interventions
Patients were divided into two groups: exercise and non-exercise groups, respectively. The exercise group–women who performed pelvic floor exercises at least three times per week during pregnancy, whereas in the postpartum period activation of the pelvic floor muscles started in the first week and continued for 6 weeks or 12 months after childbirth. The non-exercise group-women who did not do pelvic floor muscle training in the analyzed period. The women were allocated to groups after analyzing the questionnaires characterizing the frequency of exercising the pelvic floor muscles. Women who performed pelvic floor exercises less than expected in the criteria were not included in subsequent analyzes.
Outcome assessments
Three times during the study (after delivery, 6 weeks or 12 months after childbirth) women completed questionnaires aimed at evaluating the frequency and severity of urinary incontinence as well as the impact of urine leakage on the quality of life. For quantifying the intensity of urine leakage, we used a 5-point scale (0-not observed; 1-very rare (1–2 times during tested periods); 2-rare (a few times in the tested period), 3-occasionally (not more than once per week), 4-often (a few times per week); 5-very often (every day). For quantifying the impact of urine leakage on the overall quality of life, we used a 5-point scale which asked women to how much incontinence had negatively impacted upon their quality of life (scale contained signatures: 0-no influence, 1-slightly decreases; 3-decreases moderately; 5-impairs normal functioning). Moreover, we also used the UDI-6 short form and IIQ-7 questionnaires.
Covariates
The study examined the relationship between independent variables (pelvic floor exercises and perineum damage during childbirth) and dependent variables (severity of leaking urine, patients’ quality of life). We analyzed the frequency and intensity of urinary incontinence, the frequency of pelvic floor muscle training during pregnancy and the postpartum period, the impact of pelvic floor muscle exercise on urine leakage and the women’s quality of life. Moreover, we analyzed the impact of pelvic floor muscle training after episiotomy on both urine leakage and the women’s quality of life.
Statistical analyzes
After testing for the normality of distribution, data were presented as percentages for the analyzed group or as means with standard deviation (mean ± SD). Statistical analyzes were performed using Statistica 10 software, with p < 0.05. Statistical comparison was performed with the Mann–Whitney U-test, χ2 test or Student’s t-test. Analyzes of variance (ANOVA) with Tukey’s post-hoc or Kruskal–Wallis’ with Dunn’s post-hoc test were used where appropriate.
Results
Characteristics of women participating in the study were collected in Table 1.
The incidence of urinary incontinence in women during pregnancy and after childbirth
To verify the incidence of urinary incontinence among women after childbirth and to evaluate the awareness of this problem, these women were asked about both the occurrence of UI and leaking urine. According to their responses (Figure 1, white bars), during pregnancy UI occurred in 12.5% (n = 10) of women; during the postpartum period to six weeks this value increased to 16.25% (n = 13), while during the first 12 months the number decreased to 10.00% (n = 8). When questioned whether they had noted any incidents of losing urine, even a one-time incident, and the respondents’ answers differed significantly from those in the first questionnaire (Figure 1, black bars). An incident of leaking urine was reported by 36.25% (n = 29) of pregnant women, and this number increased to 45% (n = 36) during the first six weeks after delivery. After the postpartum period and up to 12 months, 26.25% (n = 21) of women complained of this symptom. The above compilation shows that a significant proportion of respondents did not identify incidents of leaking urine as UI.
In order to further assess their awareness of UI, women were asked whether they reported the incident of leaking urine to their doctor. The survey showed that only a small proportion of patients who experienced incidents of leaking urine decided to consult their doctor: 10.34% (n = 3) during pregnancy, 16.7% (n = 6) during puerperium and 23.81% (n = 5) up to 12 months after giving birth. These results show that women’s knowledge about UI is insufficient and further efforts to increase their awareness are necessary. There are many reasons why women are not reporting their problems with abnormal voiding during pregnancy. Research conducted as part of this study identified several possibilities. Nearly 40% (n = 10) of women believe that incidents of leaking urine are a physiological phenomenon during this period; for 23% (n = 6), it did not occur often enough to be reported to a doctor. The remaining respondents did not provide a reason for the lack of medical consultation. A similar analysis carried out for the postpartum period showed that 53.3% (n = 16) of patients believed that due to the sporadic nature of leaking urine there was no need to inform a doctor or midwife, 26.67% (n = 8) considered it normal, 13.34% (n = 4) did not know to whom to report, the remaining women gave no answer.
The application of pelvic floor exercises during pregnancy and after childbirth
Due to the prevalence of the problem of UI and the important role of pelvic floor muscles in proper continence, in this study, we focused on assessing the impact of pelvic floor exercise on the incidence of urine leakage. This study showed that pelvic floor exercises were mostly performed during pregnancy (Figure 2), 53% (n = 43). After childbirth, particularly in the postpartum period up to 6 weeks, there was an apparent decrease in the rate of pelvic floor exercise. Only 22.5% (n = 18) of puerperal women and 32.5% (n = 26) of women in the period up to 12 months after delivery reported the systematic application of these exercises.
The impact of pelvic floor exercises on the incidence and severity of UI in pregnancy
To assess the influence of pelvic floor exercises on the incidence of urine leakage, patients were divided into 2 groups. The first group consisted of women confirming the execution of pelvic floor exercises (n = 43), while the other group consisted of women who did not perform these exercises (n = 37). We evaluated the occurrence and severity of urine leakage. This study showed that urinary incontinence was significantly less often reported by patients who performed pelvic floor exercises during pregnancy (p = 0.036; Figure 3A). The correlation between the performance of exercises in pregnancy and the occurrence of urine leakage during this period shows a negative dependence, which proves the positive role of exercise in the prevention of urinary incontinence during pregnancy (rho = −0.27 p = 0.039). The next stage of our analysis was to evaluate the influence of pelvic floor exercises during pregnancy on the intensity of reported urine leakage using a 5-point scale (Figure 3B). Our studies showed a significant reduction in the severity of symptoms reported by women performing pelvic floor exercises compared to women who did not exercise (1.5 ± 0.67 vs. 2.75 ± 0.97; p = 0.041). An analysis of the correlation between the performance of exercises during pregnancy and the severity of UI showed the positive role of exercise in reducing the severity of the above symptom (rho = −0.25; p = 0.039).
The impact of pelvic floor exercises on the incidence and severity of UI after natural delivery and the impact of episiotomy / perineal tears
When analyzing our study attention should be paid to the issue of perineal tears and episiotomy during delivery; this affected 71.25% (n = 57) of the surveyed women. An analysis was performed with the aim of evaluating the application of pelvic floor exercises by women in the perinatal period, considering the issue of episiotomy / perineal tears, to verify the impact of these exercises on the incidence of UI. The analysis showed that, after childbirth, of women who in the course of their labor had suffered from a perineal tear or who had undergone episiotomy, 50.88% (n = 29) had not performed pelvic floor exercises and 68.97% (n = 20) of these developed UI (Figure 4A). Using a scale of 0–5 points, women rated the increase in the intensity of UI at 3.75 points in the postpartum period, and at 2.5 points at 12 months from giving birth (Figure 4B). In the group of women performing the exercises, UI occurred in 46.23% (n = 14; Figure 4A), and the severity of symptoms during the postpartum period was rated at 2.5 points and only 1.25 points one year after delivery (Figure 4B). Using the Spearman correlation, we determined a numerical relationship between the performance of exercises in women after episiotomy or a perineal tear, and the incidence of UI. It was noted that early-start pelvic floor muscle training can reduce the severity of UI in the postpartum period, especially in women who had undergone an episiotomy or suffered from perineal tears. The strongest correlation occurs in the period of up to 12 months from childbirth (rho = −0.23, p = 0.041). It is worth emphasizing how important exercises are in the group of women after episiotomy/perineal tears, especially as part of early prevention of UI.
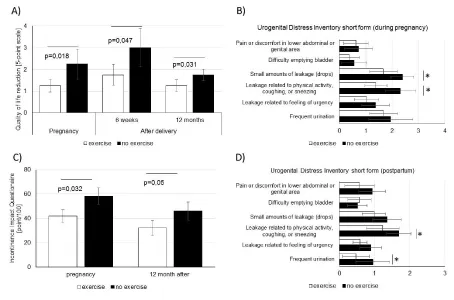
The impact of pelvic floor exercises on the quality of life of women with incidents of UI during pregnancy and after childbirth
Urinary incontinence not only influences the physiological function of the urinary system, but also significantly affects quality of life. In this study, women evaluated the impact of UI on their quality of life using a 5-point scale. We have shown that even occasional incidents of UI significantly reduce the quality of life of the women surveyed (Figure 5). Quality of life was significantly reduced both in pregnant women (2.26 ± 0.48), and in the period up to 12 months after birth (2.69 ± 0.81). Assessment of the impact of pelvic floor exercises on the quality of life of women with urinary incontinence showed a significant improvement in this parameter, especially during the postpartum period (Figure 5A). A detailed analysis performed using the UDI-6 questionnaire (Urogenital Distress Inventory-Short Form) showed that women mainly complain of discomfort associated with UI during physical activity, coughing or sneezing, frequent urination (during pregnancy) (Figure 5B) and pain and discomfort in the lower abdominal or genital area (within 12 month of delivery) (Figure 5D). The division of women into exercising and non-exercising groups allowed us to show that exercise during pregnancy significantly reduces the discomfort associated with UI during physical activity both during pregnancy (1.39 ± 0.42 vs. 2.31 ± 0.43; p = 0.048, rho = −0.21; p = 0.043) and 12 months postpartum (1.23 ± 0.48 vs. 1.69 ± 0.35; p = 0.049; rho = −0.19; p = 0.046). We also observed a significant impact of exercise on the reduction of the discomfort associated with pain in the lower abdominal or genital area during 12 months postpartum (0.93 ± 0.38 vs. 0.72 ± 0.54; p = 0.049; rho = −0.21, p = 0.043) (Figure 5D).
An analysis using the IIQ-7 questionnaire (incontinence IMPACT Questionnaire-SHORT FORM), which enables the assessment of the impact of urinary incontinence on 4 aspects of everyday life (physical activity, travel, social / relationships, emotional health), showed a significant correlation between the performance of exercises and limitations in everyday life (Figure 5C). Women exercising the pelvic floor during pregnancy rated limitations in everyday life significantly lower than inactive women (41.8 ± 5.23 vs. 57.19 ± 6.98; p = 0.032). Statistically significant effects of exercises were observed in the terms of physical activity and recreation (rho = −0.19, p = 0.041). It was also noted that training decreases feelings of depression, anger, or frustration (rho = −0.27; p = 0.049). The survey repeated after 12 months after delivery confirms that an increase in the frequency of exercise reduces limitations in the area of physical activities and recreation (rho = −0.23; p = 0.037), and also improves emotional status (rho = −0.22; p = 0.041). In general, stimulation of the pelvic floor muscles during pregnancy correlates with functional capabilities of women. It was found that training during pregnancy allows women to remain fully independent until the time of delivery.
Discussion
Taking into account the prevalence of the problem of urinary incontinence among women, it appears advisable to undertake studies allowing the evaluation of the effectiveness of available forms of physiotherapy, as well as an assessment of women’s current awareness of this important issue.
In this study, we have attempted to evaluate the impact of pelvic floor exercise on the phenomenon of UI development in women in three different periods: during pregnancy, until 6 weeks postpartum and up to 12 months after childbirth. Our studies have confirmed that UI is a common phenomenon observed in all the above groups. However, it was also noted that a significant part of the women surveyed did not identify single incidents of leaking urine as actual urinary incontinence. These results suggest that often the statistical data obtained in studies may represent an underestimation, not only due to the late reporting of women with urinary incontinence for medical consultations but also because of their inability to recognize alarming symptoms. Each incident of urine loss should be considered a potential signal of incipient dysfunction, which is the basis to make the right diagnosis and, where necessary, implement physiotherapy. Any problems associated with the leaking of urine, both during pregnancy and after childbirth, should be reported to medical personnel. Unfortunately, many women find that the above symptoms are normal during pregnancy and postpartum, which makes early implementation of appropriate therapeutic procedures impossible. According to our results, only 10.34% of women during pregnancy, 16.7% during the postpartum period and 23.81% during the 12 months after birth report the problem of UI to a gynecologist or midwife. As the reasons for not reporting this problem during pregnancy and postpartum women frequently pointed to: UI as a physiological phenomenon during this period; and the sporadic nature of the symptoms. Analyzing the above results, the duration of the symptoms has a significant impact on the decision of women to seek professional help.
The lack of an appropriate response, as well as the inability to start treatment and physiotherapy in the early stages of incontinence can significantly reduce the chances of a non-surgical solution to the problem. These studies highlight the need to educate women planning pregnancy in terms of both risk factors for urinary incontinence as well as the possibility of taking preventive actions.
In our study, we also show the beneficial effect of pelvic floor training from the perspective of UI prevention. From our study, we find that Kegel exercises had a positive impact on each of the groups. Barbara Gugała et al. [15], showed how low the level of awareness among women regarding risk factors and preventive treatment of UI was. A study published in 2014 and conducted by Park et al. [16], on a group of 510 women with UI demonstrated the positive effect of Kegel exercises in reducing the number of incidents of urine leakage. In this study, moreover, we determined the relationship between the performance of Kegel exercises by women after episiotomy or perineal tears and the occurrence of UI. It was found that training translates into a drop in the development of UI. The strongest correlation was shown within 12 months after giving birth. For comparison, Rockner [17]. Questioned 185 women four years after delivery with episiotomy and perineal tears, where UI symptoms occurred in 36% of patients. There were no significant differences in incidence between the groups. Perineal tears as well as episiotomy during childbirth cause increased risk of UI, but as we presented in our study the proper pelvic floor activation significantly reduced the frequency of UI.
The problem of UI during pregnancy was also studied by Mayer [9] and Hansen [13]. Mayer et al. [9], conducted their study on a group of 107 primiparas during pregnancy at 10 weeks and 10 months postpartum. They analyzed the incidence of UI, and the effect of natural labor and forceps delivery on the occurrence of UI. No differences were found between the two groups in terms of the frequency of incidents of leaking urine at 10 weeks and 10 months postpartum, where the incidence was an average of 32% (p = 0.3) at 10 weeks, and 20% (p = 0.6) at 10 months [9]. In their studies, Hansen et al. [13], found that UI in women during their first pregnancy was 3.3 times more frequent than in nulliparas. A year after delivery, these differences decreased to 2.5. According to our research, this problem may affect up to 45% of women in the postpartum period, and although later its incidence significantly drops, UI substantially reduces the quality of life of the surveyed women. Therefore, it should be noted that this group should be included in a special program aimed at prevention and physiotherapy of UI.
UI has a wide impact on women’s quality of life, both in terms of physical activity and psychological status. Currently, there is increasing discussion of the symptoms, risk factors and the prevention of UI. The interest in this topic among women reflects an increase in public demand for research on this phenomenon. According to our research in the context of UI, pelvic floor training is closely associated with the quality of life of women. An increase in the frequency of physical activities such as recreation leads to less trouble, thus avoids lowering life satisfaction. Physical training also helps to improve women’s mental state. Kaminska et al. [18], noted that the overall health and wellbeing of women with UI treated at Urological Clinics were rated as good by 80% of the respondents. The biggest problem for the patients were difficulties in proper performance of physical activities - 45% performed at an average level. A similar percentage of women with UI had experienced a depressed mood in the previous month. For the vast majority, UI was not an impediment to social interactions [18]. Only after a detailed analysis of this seeming insignificant health condition can we fully understand how dramatically it can affect a woman’s quality of life, especially as UI negatively impacts both the physical and psychological well-being of patients.
In summary, the phenomenon of UI has always been present; however, only the current development of public awareness has contributed to its popularization. For many years, UI was thought of as taboo and patients were afraid to seek specialist help. This problem particularly often affects pregnant and postpartum woman who are a group that needs our special attention in terms of health related quality of life. This problem particularly often affects pregnant and postpartum woman who are a group that needs our special attention in terms of health related quality of life. It seems important to note the relationship between natural delivery and the frequency of the development of UI. Our study shows the importance of educating the public about the role of prophylaxis in the prevention of UI and confirms that pelvic floor training is an effective method of prophylaxis and therapy of UI during pregnancy and postpartum period. Our study was conducted on a group of Caucasian women in childbearing age with varied socioeconomic backgrounds. As such we believe that our results and conclusions can be generalized and used for the benefit of the vast majority of women in our geographical region.
- Purc D, Rasała A (2015) Method of treating urinary incontinence. EJMT 3: 29-38.
- Abrams P, Khoury S, Wein A, eds. (1999) Incontinence: Proceedings of the 1st International Consultation on Incontinence; Monaco, June 28 ± July 1 1998. Plymouth: Health Publication Ltd 1999.
- Arrue M, Ibañez L, Paredes J, Murgiondo A, Belar M, et al. (2010) Stress urinary incontinence six months after first vaginal delivery. Eur J Obstet Gynecol Reprod Biol 150: 210–214. Link: https://goo.gl/xFG1lS
- Oblasser C, Christie J, McCourt C (2015) vaginal cones or balls to improve pelvic floor muscle performance and urinary continence in women postpartum: A quantitative systematic review. Midwifery 31: 1017-1025. Link: https://goo.gl/5H0Rxx
- Urinary Incontinence in Women. Link: https://goo.gl/IPBUHF
- Cichońska M, Maciąg D, Zboina B, Latawiec I, Krawczyk W (2013) The assessment of women’s knowledge concerning urinary incontinence. Zdrowie i dobrostan 4: 45 - 64.
- Goeschen K, Papa PP (2009) Uroginekologia zabiegowa w świetle Teorii Integralnej. Anatomia czynnościowa, diagnostyka i leczenie. Wyd. BiFolium, Lublin, 74. Link: https://goo.gl/VRBIHz
- Putowski L, Gogacz M (2007) Anatomia dna miednicy. Uroginekologia Praktyczna. Wyd. BiFolium, Lublin 29-31.
- Meyer S, Hohlfeld P, Achtari C, Russolo A, De Grandi P (2000) Birth trauma: short and long term effects of forceps delivery compared with spontaneous delivery on various pelvic floor parameters. Br J Obstet Gynaecol 107: 1360-1365. Link: https://goo.gl/dDedgp
- Miękoś E, Sosnowski M, Zydek C (2004) Risk factors and prevention of urinary incontinence in women. Przegląd Menopauzalny 5: 43-49.
- Wilson PD, Herbison RM, Herbison GP (1996) Obstetric practice and the prevalence of urinary incontinence three months after delivery. Br J Ob Gyn. 1: 154-61. Link: https://goo.gl/FKknZx
- Timur-Taşhan S, Beji NK, Aslan E, Yalçin Ö (2012) Determining lower urinary tract symptoms and associated risk factors in young women. Int J Gynaecol Obstet 118: 27–30. Link: https://goo.gl/i7K0AU
- Hansen BB, Svare J, Viktrup L, Jørgensen T, Lose G (2012) Urinary incontinence during pregnancy and 1 year after delivery in primiparous women compared with a control group of nulliparous women. Neurourol Urodyn. 31: 475–480. Link: https://goo.gl/cyGwNv
- Stadnicka G, Iwanowicz-Palus GJ (2015) the etiology of stress urinary incontinence in terms of vaginal delivery. EJMT 4: 8-15.
- Gugała B, Głaz J, Drelich A (2011) the need for patient education in the prevention of incontinence in women. Prz. Med. Uniw. Rzesz. Inst. Leków 3: 340–347.
- Park SH, Kang CB (2014) Effect of Kegel Exercises on the Management of Female Stress Urinary Incontinence: A Systematic Review of Randomized Controlled Trials. Advances in Nursing. Link: https://goo.gl/VO5v5o
- Rockner G (1999) Urinary incontinence after perineal trauma at childbirth. Scand J Caring Sci 4: 169-172. Link: https://goo.gl/x5PmDj
- Kamińska A, Kurzeja A, Ogórek-Tęcza B (2012) Jakość życia kobiet z nietrzymaniem moczu. Pielęg XXI wieku 4: 23-27. Link: https://goo.gl/l7Fcz9
Article Alerts
Subscribe to our articles alerts and stay tuned.
 This work is licensed under a Creative Commons Attribution 4.0 International License.
This work is licensed under a Creative Commons Attribution 4.0 International License.




 Save to Mendeley
Save to Mendeley
