Rheumatica Acta: Open Access
Eosinophilic Fasciitis in a Patient with Hepatitis C Virus Infection: Coincidence or Association?
Samuel Katsuyuki Shinjo* and Fernando Henrique Carlos de Souza
Cite this as
Shinjo SK, de Souza FHC (2017) Eosinophilic Fasciitis in a Patient with Hepatitis C Virus Infection: Coincidence or Association?. Rheumatica Acta: Open Access 1(1): 001-003. DOI: 10.17352/raoa.000001Eosinophilic fasciitis is a rare connective tissue disease characterized by symmetrical and painful swelling with a progressive induration and thickening of the skin and soft tissues. Its etiology is unknown, but possible causes or associated conditions include drugs, physical exercises, autoimmune diseases, neoplasia and infections.
Herein, we report, at the first time in the literature, the eosinophilic fasciitis in a patient with hepatitis C virus infection.
Introduction
Eosinophilic fasciitis is an uncommon disorder characterized by acute or subacute symmetric swelling of the skin and the subcutaneous tissues. The flanks, upper legs and forearms are usually affected, while the face and hands are spared [1-4].
The etiology of eosinophilic fasciitis is unknown, but possible causes or associated situations include drugs, extenuated physical exercises, autoimmune diseases, neoplasia and also infections [1,5-8].
However, until the present moment, there have no described cases of eosinophilic fasciitis in patient with hepatitis C virus infection.
Case Report
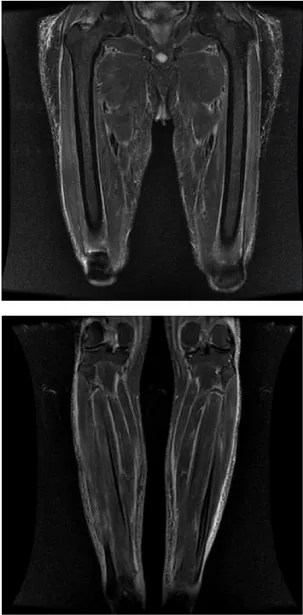
A 58 year old Caucasian male presented for evaluation of a three months history of diffuse and progressive myalgia associated with painful limitation of mobility. It evolved with lower limb edema and thickening of the forearms symmetrically (Figure 1), abdomen, and anterior neck. There was no history of Raynaud’s phenomenon, dysphagia, muscle weakness, dyspnea, sclerodactyly, ulcer cutaneous nor L-tryptophan ingestion. Patient was sedentary.
At hospital admission, the vital signs were normal. Initial laboratory tests showed peripheral blood leukocytosis (31.8x109/L) with 45.2% of white blood cells being eosinophils; creatine phosphokinase of 34U/L (reference value: 24-173U/L); aldolase of 9.6U/L (<7.5U/L); erythrocyte sedimentation rate of 23mm/1st hour (6.2-13.2mm/1st hour); C-reactive protein of 131.0mg/L (<5.0mg/L); absence of hypergammaglobulinemia; negative anti-nuclear antibody test.
Magnetic resonance imaging with evidence of thickening, symmetric edema and enhancement of the deep and superficial fascia of the thigh and legs compartments (Figure 2), without collections. Vastus lateralis muscle biopsy was performed, showing an intense area of eosinophilic inflammatory infiltration in the perimysium region, with sparse foci of inflammation in the endomysia region and necrosis of muscle fibers.
Neoplastic and parasite causes were excluded.
Additionally, patient had positive hepatitis C virus serology (HCV PCR 4355 (3.64 log), genotype 1b). The liver enzyme levels were slightly elevated and liver ultrasound was homogeneous.
Initiated prednisone 1mg/kg/day and, after 14 days, there was significant improvement of myalgia and normalization of eosinophil fraction. Subsequently, as prednisone tapering, cyclosporine was initiated at 2mg/kg/day. Concerning to the virus C infection, he was followed up on an Outpatient basis by a hepatologist.
Discussion
We report the case of a patient with eosinophilic fasciitis and hepatitis C virus infection.
Eosinophilic fasciitis is a scleroderma-like syndrome that was first described by Shulman in 1974 [1-3]. Its onset it typically acute and findings include erythema, swellivng and induration of the extremities, usually accompanied by eosinophilia, polyclonal hypergammaglobulinemia and elevated erythrocyte sedimentation rate [9-11]. Typical histologic findings include chronic inflammatory infiltration affecting deep fascia with lymphocytes, histiocytic, and occasionally eosinophils [1]. Magnetic resonance imaging can be used for the diagnosis of eosinophilic fasciitis [14-16]. The classical is the presence of fascial thickening and signal abnormalities in patients at the time of diagnosis [14,15], similarly to the present case report.
The possible causes or associated situations include drugs, extenuated physical exercises, autoimmune diseases, neoplasia [1,5-8]. Concerning to infections, there are description of eosinophilic fasciitis associated to intestinal parasitic infection [17], Mycoplasma arginini (18), tuberculosis (19) and borrelia [5,20,21]. However, until the present moment, there have no described cases of eosinophilic fasciitis in patient with hepatitis C virus infection.
The association of eosinophilic fasciitis with infectious disease [5,17-21], especially hepatitis C virus, raises the question of a real link or a fortuitous association between the conditions. We suggest that in some patients, perhaps genetically predisposed, infections may be at the origin of fasciitis.
The glucocorticoid can be considered as the first-line treatment of eosinophilic fasciitis and are usually effective in more than 70% of cases. Other treatments included non-steroid anti-inflammatory drugs, chloroquine, cimetidine, azathioprine, cyclosporine A, infliximab, PUBA and UVA-1 [12,13]. In the present case, the patient had improvement of muscle symptoms with prednisone.
In summary, we reported for the first time an eosinophilic fasciitis patient with positive serology to hepatitis C virus. Basing on other studies that describe eosinophilic fasciitis and different infections [5,17-21], the hepatitis C virus may be at the trigger of fasciitis in our patient, who must have been genetically predisposed. However, more studies with reports or a series of cases will be necessary to evaluate the exact relationship between these two entities.
- Shulman LE (1975) Diffuse fasciitis with eosinophilia: a new syndrome? Trans Assoc Am Physicians 88: 70-86. Link: https://goo.gl/5wvngK
- Rodnan GP, Di Bartolomeo A, Medsger TA Jr (1975) Proceedings: Eosinophilic fasciitis: report of six cases of a newly recognized scleroderma-like syndrome. Arthritis Rheum 18: 525. Link: https://goo.gl/EDfNum
- Andreopoulos A, Antoniou TC, Yiakoumis X, Andreopoulos G, Vaiopoulos G, et al. (2009) Eosinophilic fasciitis accompanied by serositis. Isr Med Assoc J 11: 319-320. Link: https://goo.gl/hSii6g
- Florell SR, Egan CA, Gregory MC, Zone JJ, Petersen MJ (2001) Eosinophilic fasciitis occurring four weeks after the onset of dialysis in a renal failure patient. J Cutan Med Surg 5: 33-36. Link: https://goo.gl/krJ043
- Granter SR, Barnhill RL, Duray PH (1996) Borrelial fasciitis: diffuse fasciitis and peripheral eosinophilia associated with Borrelia infection. Am J Dermatopathol 18: 465-473. Link: https://goo.gl/etT7cF
- Choquet-Kastylevsky G, Kanitakis J, Dumas V, Descotes J, Faure M, et al. (2001) Eosinophilic fasciitis and simvastatin. Arch Intern Med 161: 1456-1457. Link: https://goo.gl/G6kp2R
- Hur JW, Lee HS, Uhm WS, Jun JB, Bae SC, et al. (2005) Eosinophilic fasciitis associated with autoimmune thyroiditis. Korean J Intern Med 20: 180-182. Link: https://goo.gl/R7SsxC
- Khanna D, Verity A, Grosman JM (2002) Eosinophilic fasciitis with multiple myeloma: a new haematological association. Ann Rheum Dis 61: 1111-1112. Link: https://goo.gl/xKA5UX
- Danis R, Akbulut S, Altintas A, Ozmen S, Ozmen CA (2010) Unusual presentation of eosinophilic fasciitis: two case reports and a revie of the literature. J Med Case Report 4: 46. Link: https://goo.gl/IWkhSh
- Chun JH, Lee KH, Sung MS, Park CJ (2011) Two cases of eosinophilic fasciitis. Ann Dermatol 23: 81-84. Link: https://goo.gl/3c21Hl
- Barnes L, Rodnan GP, Medsger TA, Short D (1979) Eosinophilic fasciitis: a pathological study of twenty cases. Am J Pathol 96: 493-518. Link: https://goo.gl/9VupTK
- Weber HO, Schaller M, Metzler G, Röcken M, Berneburg M (2008) Eosinophilic fasciitis and combined UVA1-retinoid-corticosteroid treatment: two case reports. Acta Derm Venereol 88: 304-306. Link: https://goo.gl/ATvsZh
- Haiduc VF, Erkan D, Kirou K, Birchansky S, Park J, et al. (2008) Anti-neutrophil cytoplasmic antibody (c-ANCA) positive recurrent eosinophilic fasciitis responsive to cyclophosphamide: a clinical pathology conference held by the Division of Rheumatology at Hospital for Special Surgery HSS J 4: 81-86. Link: https://goo.gl/q1XcB3
- Bischoff L, Derk CT (2008) Eosinophilic fasciitis: demographics, disease pattern and response to treatment: report of 12 cases and review of the literature. Int J Dermatol 47: 29-35. Link: https://goo.gl/OBDH57
- Baumann F, Brühlmann P, Andreisek G, Michel BA, Marincek B, et al. (2005) MRI for diagnosis and monitoring of patients with eosinophilic fasciitis. AJR Am J Roentgenol 184: 169-174. Link: https://goo.gl/VwCi32
- Agnew KL, Blunt D, Francis ND, Bunker CB (2005) Magnetic resonance imaging in eosinophilic fasciitis. Clin Exp Dermatol 30: 435-436. Link: https://goo.gl/o56BYr
- Oliveira M, Patinha F, Marinho A (2016) Eosinophilic fasciitis after parasite infection. Reumatologia 54: 38-41. Link: https://goo.gl/bPsJxC
- Silló P, Pintér D, Ostorházi E, Mazán M, Wikonkál, N et al. (2012) Eosinophilic fasciitis associated with Mycoplasma arginine infection. Clin Microbiol 50:1113-1117. Link: https://goo.gl/Ao4HPy
- Roca B, Bennasar MA, Pitarch A (2005) Miliary tuberculosis in a patient with eosinophilic fasciitis. South Med J 98:107-10. Link: https://goo.gl/Ja6D8o
- Belot V, Mulleman D, Perrinaud A, Abdallah-Lotf M, Machet MC, et al. (2007) Eosinophilic fasciitis associated with Borrelia burgdorferi infection. Ann Dermatol Venereol 134: 673-677. Link: https://goo.gl/t8x6W9
- Kikuchi O, Murai H, Ikezoe K, Kawajiri M, Ohyagi Y, et al. (2004) Eosinophilic fasciitis associated with Borrelia afzelii infection. Rinsho Shinkeigaku 44: 299-302.. Link: https://goo.gl/Lm4y9j
Article Alerts
Subscribe to our articles alerts and stay tuned.
 This work is licensed under a Creative Commons Attribution 4.0 International License.
This work is licensed under a Creative Commons Attribution 4.0 International License.

 Save to Mendeley
Save to Mendeley
