Are Leukocyte Esterase (LE) strip and Alpha-Defensin kit reliable enough to diagnose peri-prosthetic joint infection, intra-operatively?
1Consultant Orthopedic Surgeon, Orthopedic Department, Lahore General Hospital, Pakistan
2Assistant Professor Orthopedic Surgery, Lahore General Hospital, Pakistan
3Consultant Orthopedic Surgery, Lahore General Hospital, Pakistan
4Head of Department of Orthopedic Surgery, Lahore General Hospital, Pakistan
5Ex-Head of Department of Orthopedic Surgery, Lahore General Hospital, Pakistan
Author and article information
Cite this as
Gill UN, Hamid A, Uddin S, Shair NA, Qasim M, et al. (2022) Are Leukocyte Esterase (LE) strip and Alpha-Defensin kit reliable enough to diagnose peri-prosthetic joint infection, intra-operatively?. Rheumatica Acta: Open Access. 2022; 6(1): 001-005. Available from: 10.17352/raoa.000014
Copyright License
© 2022 Gill UN, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.Background: Despite improvement in sterilization techniques, peri-prosthetic joint infection (PJI) is the most fearsome complication after hip and knee arthroplasties. Various strategies have been devised from time to time to diagnose and treat PJI. Recently, Leukocyte esterase and alpha-defensin are identified as markers of active infection in synovial fluid. Therefore, kits are designed to detect these two markers during surgery. If found reliable, these tests will increase the confidence of surgeons in situations, where the diagnosis of PJI is not established.
Material and methods: This study was conducted on 132 patients in Lahore General Hospital; from August 2020 to December 2021. Leukocyte Esterase strip and Alpha-Defensin kit were used to detect infection in synovial samples taken just before performing arthrotomy, intra-operatively. Patients were divided into 2 groups, Group-A had 31 patients with peri-prosthetic joint infection (PJI) diagnosed as per Musculoskeletal Infection Society (MSIS) criteria, whereas in Group B 101 patients were present in whom PJI was not present. Synovial tissue and fluid samples were also sent to a laboratory for culture and histopathology; so that sensitivity and specificity of LE strips and Alpha-Defensin Kits could find out.
Results: The mean age of patients in our study was 59.6 SD 11.90 years with a male to female ratio of 85:47. 31 patients were diagnosed as PJI after primary hip or knee arthroplasty based on serological investigations and culture of joint aspiration. The sensitivity and specificity of LE strips were 90.32% and 95.04%, whereas that of Alpha defensin was 93.54% and 100% respectively. The correlation coefficient between the LE strip test and synovial fluid polymorphonuclear neutrophils (PMN) counts was 0.811 and it was even higher when the Alpha-Defensin kit was used (0.845).
Conclusion: Both LE and Alpha-Defensin kits are highly specific and sensitive in diagnosing PJI. Though Alpha-defensin is more accurate the cost-effectiveness of the LE strip makes it a more feasible option in diagnosing PJI, intra-operatively.
Arthroplasty remains the best option to treat various joint pathology like advanced osteoarthritis [1], as it improves the quality of life by relieving pain, increasing range of motion, correcting deformities, and making patients more independent to carry out daily life activities [2]. This is the reason that in 2016, 87% of patients suffering from advanced osteoarthritis were treated by knee arthroplasty; and it is expected that by the year 2030, the number of patients will increase by 600% [3]. With this increase in the number of procedures comes complications. Out of all the complications, peri-prosthetic joint infection is the worst. In the USA in the year 2009, 2.4% of all joint replacement surgeries got infected [4]. According to various sources, 1%-3% of all replacement surgeries got infected worldwide [5,6].
Various criteria are designed to diagnose PJI. Musculoskeletal Infection Society (MSIS) introduced the criteria in 2011. There are two major and six minor components of this criteria. The presence of either of the two major or four out of six minor criteria is required for the diagnosis of PJI. The two major criteria are the presence of a sinus that is communicating with the prosthesis and the presence of the same pathogen on two positive cultures taken from synovial fluid or surrounding tissue. Six minor points are i) increased level of CRP(>10mg/L) and ESR(>30mm/h), ii) Increased number of white blood cells in synovial fluid ( >3000 cells/µL), iii) Increased percentage of Polymorphogenic neutrophils PMN (>65%) in synovial fluid, iv) Presence of purulence in synovial fluid, v) presence of five or more neutrophils on at least five high-power fields in frozen section analysis and vi) positive culture of synovial fluid or tissue [7].
Though widely acceptable, MSIS criteria for PJI has some flaws. ESR and CRP are sometimes misleading especially after the first stage of revision surgery, in individuals taking antibiotics, in patients with delayed or low-grade infections, etc. Frozen sections are usually not taken routinely and it is a time-consuming procedure that requires a special setup with multiple medical disciplines involved. Lastly, sometimes it is not possible to aspirate synovial fluid from joints like the hip joint for histopathological examination and culture. So there is an increasing need for simple, cheap, less time-consuming tests for the diagnosis of PJI. The first alteration that was made in MSIS criteria was made by the International Consensus Group on PJI in 2013 [8]. This group included the Leukocyte Esterase test as a minor criterion in place of WBC count in synovial fluid. In 2018, PJI was re-defined by a multi-centric retrospective study, which included alpha-defensin as an important component of minor criteria. There are ongoing studies on various markers for the diagnostic markers for PJI, that include serum D-dimer level [9] synovial C-reactive protein (CRP) [10,11] and molecular techniques such as next-generation sequencing [12].
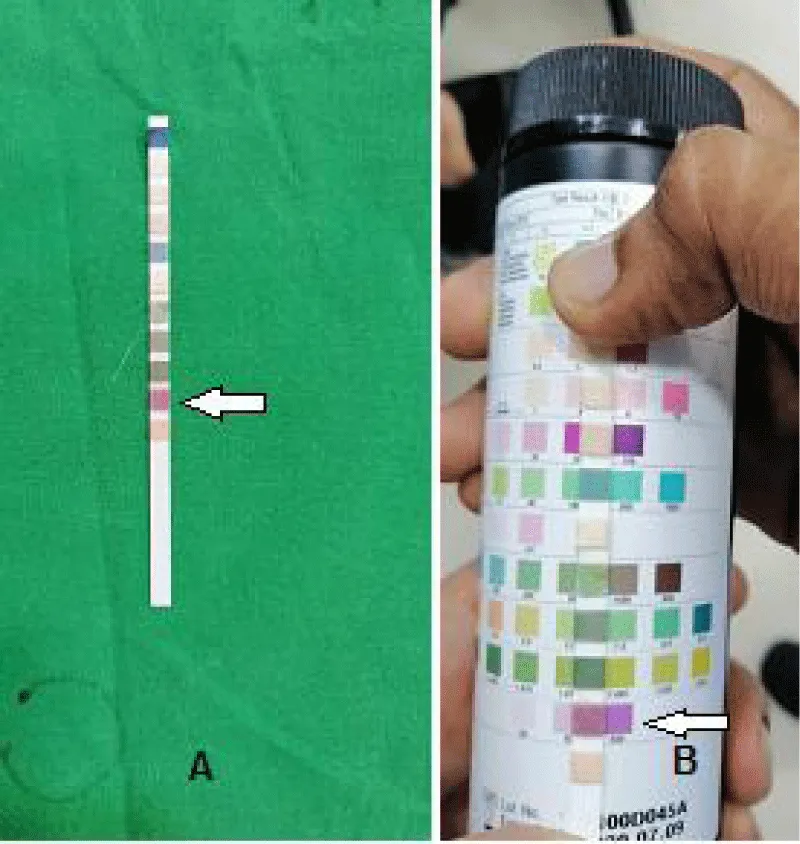
Leukocyte Esterase (LE) strips were initially used for Pyuria. Leukocyte Esterase is the enzyme that is secreted by Neutrophil [13]. The presence of this marker turns LE strips from white to light and ultimately to dark purple color. Recently these strips were used to diagnose PJI and because of their efficacy it was included in MSIS minor criteria. LE strips are cheap and the test requires a few drops of synovial fluid and it requires a couple of minutes to indicate the result. Alpha-defensin is a part of the immune system which is released by neutrophils in response to pathogens and destroys the membrane of a pathogen [14]. Alpha-defensin is detected by either a laboratory-based ELIZA test or by an Alpha-defensin test kit. The main advantage of these two tests is that they have a high level of sensitivity and specificity [15], they require not more than a few minutes to indicate results and these tests can be performed in the operation theater, during surgery by the surgeon himself.
Despite the benefits of these tests, they are not frequently used by surgeons in Pakistan. This study is designed to establish the effectiveness of these two tests so that early diagnosis of PJI be made and timely steps are taken by Orthopedic surgeons in Pakistan.
Materials and methods
In this prospective study, we performed alpha-defensin and LE strip tests on 132 patients, who were either undergoing the first or second stage of revision joint surgeries from August 2020 to December 2021, in Lahore General Hospital. To have a better understanding of the results, we divided patients into two groups. Group-A had 31 patients with peri-prosthetic joint infection (PJI) diagnosed according to Musculoskeletal Infection Society (MSIS) criteria, whereas in Group B 101 patients were present in whom PJI was not present.
Procedure
During surgery, just before arthrotomy, two 10cc syringes were used to aspirate synovial fluid; one for alpha-defensins and LE strip tests, and the second syringe was sent to the laboratory for culture and histopathology. After aspiration, a single drop of synovial fluid was applied to the LE strip, under aseptic conditions, while the rest of the sample was used for an alpha defensin test kit. Three drops from prefilled dropper bottle were put on the test device. It takes 2 to 3 minutes for the LE strip and 10 minutes for the alpha-defensin kit to give the final result. LE pad changes its color from white to light purple to dark purple which is considered positive (Figure 1). Whereas, two lines on the alpha defensin kit`s test device show a positive result (Figure 2).
Patients who presented after primary arthroplasty (Hip or knee) with unexplained pain, loosening (aseptic/septic), swelling around replaced joint, diagnosed as PJI by serological studies were included in this study. Also, the patients who were candidates of second stage revision arthroplasties, with serological signs of no active infection and negative culture report of synovial aspiration were included in this study.
Data analysis
Data was entered and analyzed using SPSS 23. Quantitative data like age is presented by mean and standard deviation. Qualitative data like gender, hip or knee replacement, etc are presented in percentages. Results from both tests were compared with each other, as well as with the Laboratory culture report. Also, the results were compared with synovial fluid WBC and neutrophil counts. Sensitivity, specificity, and Positive and Negative predictive values were calculated using the following formulas:
Sensitivity=[A/(A+C)]×100
Specificity=[D/(B+D)]×100
Positive predictive value(PPV)=[A/(A+B)]×100
Negative predictive value(NPV)=[D/(C+D)]×100
Results
The mean age of patients in our study was 59.6 +/- 11.90 years (Range: 48-75 years). The male to female population was 85:47. 31 patients were diagnosed as PJI after primary hip or knee arthroplasty based on serological investigations and culture of joint aspiration (Table 1).
The sensitivity and specificity of LE strips were 90.32% and 95.04%, whereas the Positive Predictive Value (PPV) and Negative Predictive Value (NPV) were 84.84 and 96.96 respectively, as shown in Table 2.
The sensitivity and specificity of Alpha defensin were 93.54% and 100% respectively with a Positive Predictive Value (PPV) and Negative Predictive Value (NPV) of 100 and 98.05, as shown in Table 3.
Discussion
After joint replacement surgery, the diagnosis of periprosthetic joint infection is still a matter of debate, because serological markers like ESR and CRP are sometimes misleading. So MSIS came out with the criteria to diagnose PJI. But this criteria was also time and resources consuming because the culture of a causative organism takes a week or so [16,17]. To answer these shortcomings some modifications were made to MSIS criteria in the year 2013. Two tests were included in this criteria which are the Leukocyte Esterase strip test and alpha-defensins lateral flow kit. Both of these tests consume virtually no time, can be performed intra-operatively, do not require special gadgets, and give the surgeon idea about the presence or absence of infection.
Various studies have shown a high degree of sensitivity and specificity of the LE strip test. These strips were being used to diagnose UTIs for the past thirty years or so, but Parvizi, et al. [13] identified their use in diagnosing PJI. Since then many western studies were conducted to establish its efficacy. In a study by De Vecchi, et al. [18] this test was positive in 25 out of 27 infected arthroplasties and was negative in 99 out of 102 not infected arthroplasties with a sensitivity of 92.6% and specificity of 97.0%. In our study, the sensitivity and specificity of LE strips were 90.32% and 95.04%. Similar results were obtained in studies by Aggarwal, et al. [19] Wetters, et al. [20] Nelson, et al. [21] Colvin, et al. [22]. The only issue we faced with this test was the difference between observers in matching the strip colour with that of the given reference colours in few cases. But this problem was solved by nominating five observers to match the colours of the LE strip with the reference colour and the decision of the majority was considered final. Moreover, in our study, there was no need to centrifuge the synovial fluid sample because we took the samples before arthrotomy using a 10 cc syringe, with virtually no contamination of synovial fluid with blood. Moreover, there was a strong association of synovial fluid WBC and Neutrophil count with that of LE strips result of our study. We found that the correlation coefficient between the LE strip test and synovial fluid polymorphonuclear neutrophils (PMN) counts was 0.811 and it was even higher when the Alpha-Defensin kit was used (0.845). Similar results were shown by the study of Chi-Wang, et al. [23] In his study, the correlation coefficient between the LE strip test and synovial fluid WBC and PMN counts were 0.578 and 0.845 which are significant.
Alpha-defensins are released by Neutrophils in response to pathogens which shows that this peptide is only present in the synovial fluid of the infected joint and not in other inflamed joints which mimic PJI. So there are two methods of detecting this peptide. One is through laboratory (ELIZA) which is regarded as better than the second method [24]. The second technique is the Alpha defensin lateral flow kit. Some studies show excellent results in diagnosing PJI with these kits. In a study by Gehrke, et al. [25] on 195 cases, the overall sensitivity of this test was 92.1% and specificity was 100% with the positive predictive value of 100% as this peptide is present only in infected joints and the negative predictive value was 95.2%. Thus overall accuracy of this test was 96.9%. In our study sensitivity and specificity of Alpha, and defensin was 93.54% and 100% respectively. Alpha defensin lateral flow kit showed excellent sensitivity, and specificity but the only issue with this test is the cost of this kit. But the usefulness of this kit in giving the operating surgeon a clear picture of PJI there and then is something worth this expense.
Conclusion
Both LE and Alpha-Defensin kits are highly specific and sensitive in diagnosing PJI. Though Alpha-defensin is more accurate the cost-effectiveness of the LE strip makes it a more feasible option in diagnosing PJI, intra-operatively.
- Fingar KR, Stocks C, Weiss AJ, Steiner CA. Most Frequent Operating Room Procedures Performed in US Hospitals. Agency for Healthcare Research and Quality (US); 2014; 1–15.
- Hunter DJ. Pharmacologic therapy for osteoarthritis--the era of disease modification. Nat Rev Rheumatol. 2011 Jan;7(1):13-22. doi: 10.1038/nrrheum.2010.178. Epub 2010 Nov 16. PMID: 21079644.
- Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007 Apr;89(4):780-5. doi: 10.2106/JBJS.F.00222. PMID: 17403800.
- Bozic KJ, Kurtz SM, Lau E, Ong K, Vail TP, Berry DJ. The epidemiology of revision total hip arthroplasty in the United States. J Bone Joint Surg Am. 2009 Jan;91(1):128-33. doi: 10.2106/JBJS.H.00155. PMID: 19122087.
- Kurtz SM, Lau E, Watson H, Schmier JK, Parvizi J. Economic burden of periprosthetic joint infection in the United States. J Arthroplasty. 2012 Sep;27(8 Suppl):61-5.e1. doi: 10.1016/j.arth.2012.02.022. Epub 2012 May 2. PMID: 22554729.
- Jämsen E, Varonen M, Huhtala H, Lehto MU, Lumio J, Konttinen YT, Moilanen T. Incidence of prosthetic joint infections after primary knee arthroplasty. J Arthroplasty. 2010 Jan;25(1):87-92. doi: 10.1016/j.arth.2008.10.013. Epub 2008 Dec 4. PMID: 19056210.
- Parvizi J, Zmistowski B, Berbari EF, Bauer TW, Springer BD, Della Valle CJ, Garvin KL, Mont MA, Wongworawat MD, Zalavras CG. New definition for periprosthetic joint infection: from the Workgroup of the Musculoskeletal Infection Society. Clin Orthop Relat Res. 2011 Nov;469(11):2992-4. doi: 10.1007/s11999-011-2102-9. PMID: 21938532; PMCID: PMC3183178.
- International Consensus on Periprosthetic Joint Infection. 2013.
- Shahi A, Kheir MM, Tarabichi M, Hosseinzadeh HRS, Tan TL, Parvizi J. Serum D-Dimer Test Is Promising for the Diagnosis of Periprosthetic Joint Infection and Timing of Reimplantation. J Bone Joint Surg Am. 2017 Sep 6;99(17):1419-1427. doi: 10.2106/JBJS.16.01395. PMID: 28872523.
- Tetreault MW, Wetters NG, Moric M, Gross CE, Della Valle CJ. Is synovial C-reactive protein a useful marker for periprosthetic joint infection? Clin Orthop Relat Res. 2014 Dec;472(12):3997-4003. doi: 10.1007/s11999-014-3828-y. Epub 2014 Jul 29. PMID: 25070920; PMCID: PMC4397770.
- Omar M, Ettinger M, Reichling M, Petri M, Guenther D, Gehrke T, Krettek C, Mommsen P. Synovial C-reactive protein as a marker for chronic periprosthetic infection in total hip arthroplasty. Bone Joint J. 2015 Feb;97-B(2):173-6. doi: 10.1302/0301-620X.97B2.34550. PMID: 25628278.
- Tarabichi M, Shohat N, Goswami K, Alvand A, Silibovsky R, Belden K, Parvizi J. Diagnosis of Periprosthetic Joint Infection: The Potential of Next-Generation Sequencing. J Bone Joint Surg Am. 2018 Jan 17;100(2):147-154. doi: 10.2106/JBJS.17.00434. PMID: 29342065.
- Parvizi J, Jacovides C, Antoci V, Ghanem E. Diagnosis of periprosthetic joint infection: the utility of a simple yet unappreciated enzyme. J Bone Joint Surg Am. 2011 Dec 21;93(24):2242-8. doi: 10.2106/JBJS.J.01413. PMID: 22258769.
- Lehrer RI, Ganz T. Defensins: endogenous antibiotic peptides from human leukocytes. Ciba Found Symp. 1992;171:276-90; discussion 290-3. doi: 10.1002/9780470514344.ch16. PMID: 1302183.
- Bonanzinga T, Zahar A, Dütsch M, Lausmann C, Kendoff D, Gehrke T. How Reliable Is the Alpha-defensin Immunoassay Test for Diagnosing Periprosthetic Joint Infection? A Prospective Study. Clin Orthop Relat Res. 2017 Feb;475(2):408-415. doi: 10.1007/s11999-016-4906-0. PMID: 27343056; PMCID: PMC5213924.
- Tsaras G, Maduka-Ezeh A, Inwards CY, Mabry T, Erwin PJ, Murad MH, Montori VM, West CP, Osmon DR, Berbari EF. Utility of intraoperative frozen section histopathology in the diagnosis of periprosthetic joint infection: a systematic review and meta-analysis. J Bone Joint Surg Am. 2012 Sep 19;94(18):1700-11. doi: 10.2106/JBJS.J.00756. PMID: 22992880.
- Deirmengian C, Kardos K, Kilmartin P, Cameron A, Schiller K, Parvizi J. Diagnosing periprosthetic joint infection: has the era of the biomarker arrived? Clin Orthop Relat Res. 2014 Nov;472(11):3254-62. doi: 10.1007/s11999-014-3543-8. PMID: 24590839; PMCID: PMC4182392.
- De Vecchi E, Villa F, Bortolin M, Toscano M, Tacchini L, Romanò CL, Drago L. Leucocyte esterase, glucose and C-reactive protein in the diagnosis of prosthetic joint infections: a prospective study. Clin Microbiol Infect. 2016 Jun;22(6):555-60. doi: 10.1016/j.cmi.2016.03.020. Epub 2016 Mar 31. PMID: 27040804.
- Aggarwal VK, Tischler E, Ghanem E, Parvizi J. Leukocyte esterase from synovial fluid aspirate: a technical note. J Arthroplasty. 2013 Jan;28(1):193-5. doi: 10.1016/j.arth.2012.06.023. Epub 2012 Aug 3. PMID: 22868070.
- Wetters NG, Berend KR, Lombardi AV, Morris MJ, Tucker TL, Della Valle CJ. Leukocyte esterase reagent strips for the rapid diagnosis of periprosthetic joint infection. J Arthroplasty. 2012 Sep;27(8 Suppl):8-11. doi: 10.1016/j.arth.2012.03.037. Epub 2012 May 17. PMID: 22608686.
- Nelson GN, Paxton ES, Narzikul A, Williams G, Lazarus MD, Abboud JA. Leukocyte esterase in the diagnosis of shoulder periprosthetic joint infection. J Shoulder Elbow Surg. 2015 Sep;24(9):1421-6. doi: 10.1016/j.jse.2015.05.034. PMID: 26279499.
- Colvin OC, Kransdorf MJ, Roberts CC, Chivers FS, Lorans R, Beauchamp CP, Schwartz AJ. Leukocyte esterase analysis in the diagnosis of joint infection: can we make a diagnosis using a simple urine dipstick? Skeletal Radiol. 2015 May;44(5):673-7. doi: 10.1007/s00256-015-2097-5. Epub 2015 Jan 29. PMID: 25626524.
- Wang C, Li R, Wang Q, Duan J, Wang C. Leukocyte Esterase as a Biomarker in the Diagnosis of Periprosthetic Joint Infection. Med Sci Monit. 2017 Jan 21;23:353-358. doi: 10.12659/msm.899368. PMID: 28108745; PMCID: PMC5382836.
- Suen K, Keeka M, Ailabouni R, Tran P. Synovasure 'quick test' is not as accurate as the laboratory-based α-defensin immunoassay: a systematic review and meta-analysis. Bone Joint J. 2018 Jan;100-B(1):66-72. doi: 10.1302/0301-620X.100B1.BJJ-2017-0630.R1. PMID: 29305453.
- Gehrke T, Lausmann C, Citak M, Bonanzinga T, Frommelt L, Zahar A. The Accuracy of the Alpha Defensin Lateral Flow Device for Diagnosis of Periprosthetic Joint Infection: Comparison with a Gold Standard. J Bone Joint Surg Am. 2018 Jan 3;100(1):42-48. doi: 10.2106/JBJS.16.01522. PMID: 29298259.
Article Alerts
Subscribe to our articles alerts and stay tuned.
 This work is licensed under a Creative Commons Attribution 4.0 International License.
This work is licensed under a Creative Commons Attribution 4.0 International License.

 Save to Mendeley
Save to Mendeley
