Archives of Nursing Practice and Care
A Study of Reliability and Validity an Attitude Scale towards Simulation-Based Education
Gul Pinar1*, Gokce Banu Acar1 and Adnan Kan2
2Gazi University, Faculty of Education Department of Science Education, Ankara, Turkey
*Corresponding author: Gul Pinar, Nursing Department, Yildirim Beyazit University Faculty of Health Sciences, Ankara, Turkey, 06500, Teknikokullar, Ankara, Turkey, Tel:+ 9(0)3123241501; E-mail: [email protected]
Cite this as
Pinar G, Acar GB, Kan A (2016) A Study of Reliability and Validity an Attitude Scale towards Simulation-Based Education. Arch Nurs Pract Care 2(1): 028-031. DOI: 10.17352/2581-4265.000010Aim: The aim of the current study was to develop a scale to measure the attitudes of nursing students towards simulation-based education.
Method: In the 2014-2015 academic years, a total of 165 nursing students participated to the study in Ankara from 8 nursing schools. The Scale consisted of 38 items to be graded by 5 point Likert type. Cronbach alpha internal reliabilit, Kendall W test, Kaiser Meyer Olkin test, Barlett’s test and exploratory factor analysis were used to analyze the validity and reliability o the scale.
Results: The Scale consisted of 38 items to be graded by 5 point Likert type. The result of the analysis provided four factors structure for the scale. (1. satisfaction – self-confidence, 2. clinical competency – self-efficacy, 3. seriousness - fidelity, 4. barriers – difficulties). Corrected item-total correlation values of the scale items varied between 0.59-0.76. The reliability coefficient was found as Crα=0.72. It was determined that the scale could categorize students for their attitude levels (p<0.001).
Conclusion: Findings of the research indicate that the scale has good psychometric properties.
Introduction
The professional education centers, with their new techniques and equipment, offer unique opportunities for dynamic, complex, and critical situations to be experienced and managed [1,2]. In the nursing education the psychomotor skills are acquired at the professional skills laboratory. Simulation is gaining popularity as a means to provide innovative clinical learning experiences that bridging the gap between theory and practice in nursing education [3,4]. The growing complexities of patient care require nurses to master not only knowledge and procedural skills but also the ability to effectively communicate with patients, relatives, and other health care providers and also to coordinate a variety of patient care activities [5,6]. Simulation experience offers a unique opportunity to educate students for master the skills of clinical judgment, competency, self-confident, communication, delegation, conflict management, decision-making, ethical dilemmas and critical thinking skill without jeopardizing patient safety [4,7].
Simulations range from simple to complex (task trainer, virtual reality, web-based simulation basic mannequin simulators; low, moderate and high fidelity simulators, life-like human mannequin that breathes, blinks, talks, and has heartbeat, pulse and lung sounds). Especially, recent advances in technology have potentially changed the definition of simulation by way of doing repetitive exercises in each skill area [5]. This simulator can be used for scenarios from simple physical examination to interdisciplinary major trauma management. These scenarios should be realistic, practical, and comprehensive. There must also be provision for video recording equipment and sufficient space for equipment setup. After simulation scenario, the educator and the student should participate in an active debriefing [8]. Each simulation session should also include an evaluation of the overall experience by student. Simulation approaches not only to help students to attain educational goals but also to enhance nursing practice and teaching methodology for educators [7]. Effective evaluation of simulation experience have been identified as essential components of simulation-based training. Although use of simulation in nursing education has increased, concrete research is lacking, with many studies resulting in students’ attitude and perceptions towards simulation.
Aim
The aim of this study was to develop a scale for determining attitudes of nursing students towards simulation-based education (SBE).
Material and Methods
Type of research
This study has been designed as a methodological study.
Study group
The study was conducted by a total of 165 nursing students with simulation experience who were 3rd or 4th year students during the 2014-2015 school year. 18.8% (n=31) of the study group were male, and 81.2% (n=134) were female. Required institutional approvals were granted prior to the study. 1st and 2nd year nursing students do not have any previous simulation-based learning experiences. Therefore they were not involved in our study.
Inclusion criteria: The inclusion criteria for the students in the current study were (a) that the students did attend any course regarding simulation at a university (b) that he or she agreed to participate and (c) that students enrolled in the nursing program.
Exclusion criteria: Nursing students who were under the age 18, and those who did not volunteer to be in the study.
Writing and testing of scale Items
We have rewieved the literature regarding “attitude” measurements first while creating items regarding Simulation Based Education Attitude Scale (SBEAS). We have taken aspect suitable for the construct regarding attitude (statements in attitude sentences, their contents etc.) and conceptual equivalence (cognitive, affective, and behavioral) into consideration. According to literature review, SBEAS at national and international levels were not found, only studies on graduation levels of students following simulation and validity studies for simulation evaluation forms with which suggestions were given were found. By drawing from the literature, we have prepared 50 items regarding SBEAS [6,9-12]. For the validity of the scale, we have taken three expert opinions and suggestions for each statement. In this regard, a form comprised of 38 items was created after 12 out of 50 items were discarded as they were found to be unintelligible. Students filling out the scale had expressed their opinions on a 5 point Likert scale ranging from completely agree [5], to completely disagree [1].
Using the data gathering tool
A pilot scheme was applied to 15 nursing students in 3rd or 4th year who have volunteered to the research on the scale we’ve created. Items were found to be intelligible in general, and the scale was completed in 10 minutes. The final 38 item form of the scale was filled out by 175 nursing undergraduates. However, the study was comprised of 165 students as some of the scales were not complete.
Data analysis
Item statistics and internal consistency of sub dimensions were evaluated in the study regarding reliability of SBEAS. We have used the Kaiser-Meyer Olkin (KMO) coefficient and the Barlett Sphericity test in factor analysis. Following creation of factor constructs, we have named them and used the Cronbach Alpha (Crα) reliability test.
Findings
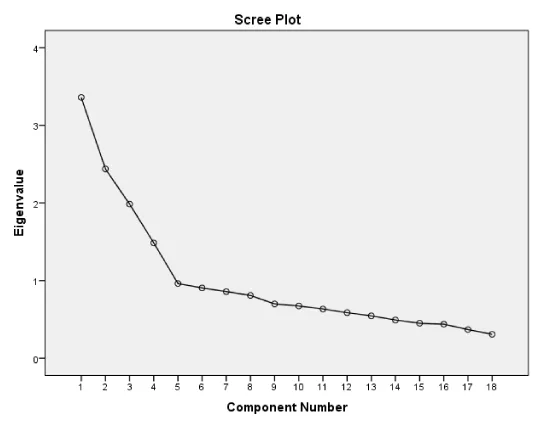
We have used the “rotated principal components analysis” in order to obtain information regarding structural validity of the scale. Suitability of the data to principal components analysis was conducted using the KMO coefficient. According to this, the data is suitable for the analysis when the KMO coefficient gets closer to 1, and it’s a perfect match if it is 1. We have determined whether the data comes from multivariate normal distribution (χ2=656,417; p<0,05). It was found that the sample size was sufficient, the data was suitable for factor analysis and items were correlated to conduct a factor analysis on the findings of the Barlett test. Following the factor analysis, 20 out of 38 items were removed as they were not correlated with other items. A construct with 4 sub factors with an eigenvalue of over 1 each was created using the remaining 18 items (Table 1, Figure 1). This has increased the Crα value from 0.70 to 0.72.
Satisfaction - Self-Confidence [1-6]: The eigenvalue of the first factor which provides information regarding significance level and weight of each factor within this construct was found to be 3.36. This sub-factor alone explains 18.66% of the attitude variable.
Clinical Competence - Self-Efficacy [7-11]: The eigenvalue of this factor was found to be 2.43. This sub-scale (factor) alone explains 13.55% of variance of relevant attitude variable.
Seriousness - Fidelity [12-15]: The eigenvalue of this factor was found to be 1.98. This factor alone explains 11.03% of variance of relevant attitude variable.
Barriers - Difficulties [16-18]: The eigenvalue of this factor was found to be 1.48. This factor alone explains 8.25% of variance of relevant attitude variable. These three factors explain 51% of variance regarding relevant attitude variable.
Factor loads of the items included in the scale range between 0.59 and 0.76 (Table 1). All of these findings were used a proof that the scale has a construct validity at a sufficient level. Items test correlations regarding item validity and homogeneity of the scale were calculated. All of these findings show that the items have high internal consistency and are valid and reliable.
Regarding reliability of the scale, the Crα reliability coefficients of the whole scale and each sub dimension were calculated separately (Table 2). Regarding reliability and homogeneity of the scale, Crα reliability and item test correlations were calculated. The Crα reliability of the whole scale was 0.722, Crα regarding the first factor was 0.739, Crα regarding the second sub factor was 0.657, Crα regarding the third sub factor was 0.631, and Crα regarding the fourth sub factor was 0.625. All of these findings were used a proof that the scale has a reliability at a sufficient level.
As apparent in Table 3, correlation between scores obtained from SBEAS and scores obtained from sub factors were between 0.33 and 0.71 and these correlation coefficients were found to be significant at the 0.01 level. The fact that these correlations were significant shows that these four sub factors are SBEAS components.
Discussion
The best learning for adult education can be obtained by active participation in the education process and taking a role in the education process. Nursing is an occupation that requires building of psychomotor and behavioral skill in addition to cognitive skills and therefore has been largely affected from fast paced developments in the field of science and technology [1-3]. Nursing students must trained in leadership, teamwork, evidenced-based practice, open communication, learning from mistakes for their actions [13]. Simulation, as one of these methods, provides a means to learn based on experience increases students’ knowledge levels and self-confidence and enables development of clinical decision-making skills [14,15]. In a study by Pınar and Doğan on nursing undergraduates, the simulation model was found to be beneficial as it shortens the learning period, and develops motivation and feelings of confidence [9]. In a study by Ross et al., on nursing undergraduates, it has found that students undergoing simulation based education prior to clinical practices are largely satisfied with their education, they provide benefits to patients, they are accepted by clinical nurses, and they enjoy an increase in their level of knowledge [13]. Dieckmann and Ganley & Linnard-Palmer [19], defined that simulation may cause a high level of stress and anxiety because of the unfamiliarity in the learning approaches used and hesitation towards the risk of exposure of one’s incompetency [16,17]. Use of the simulation model gets more common during the process of preparing nursing students to the clinical environment, although we were not able to find a study in which student attitudes towards simulation based education. In fact, nurse educators should assess the students’ knowledge; skills and attitudes about simulation education to provide quality of care. In addition educators need more information about how to best optimize simulation as teaching method [4]. In 2006, the National League for Nursing developed. The Simulation Design Scale to evaluate students’ reactions, beliefs about self-confidence, satisfaction, scenario design, and educational practices associated with simulation [6]. Recently, many researchers, administrators and educators become involved with simulation outcomes [7]. In a study, findings present that all undergraduate students improved their performances towards teamwork concepts after simulation-based experience [10]. In this study, we think that proving validity and reliability of SBEAS, which would enable evaluation and development of SBE programs, would benefit the literature greatly. Also, evaluating the results of SBE which has arisen from the need for innovation in technology and education, would provide a standard approach for both student development and development of institutes and teachers.
Conclusion and Recommendation
The SBEAS provides a reliable and construct valid measure of student perceptions of and attitudes toward simulation-based education. In this study, we have done validity and reliability regarding measurement of attitudes of nursing students towards SBE and developed a tool that is comprised of 18 items and 4 sub dimensions. The Crα for the whole scale was 0.722, we think that this scale can be used for evaluating students’ attitudes towards simulation education in a reliable manner. As a result, measuring features of students’ attitudes towards simulation education by using the correct approach established for education can contribute to evaluation and development of education. If this scale is going to be used for healthcare professionals other than nursing students, we suggest repeating validity and reliability studies on larger groups based on data obtained from such groups.
The first limitation of this study is that we selected a convenience sample from university. This study was on simulation experiences of 3rd and 4th grade students, so it has been conducted on volunteer students within such groups. Despite this limitation, our sample size allowed us to randomly select separate confirmatory and exploratory subsamples for the conduct of confirmatory and when indicated exploratory factor analysis. Also, we think that it would contribute to the literature greatly, as it is the first scale that evaluates attitudes of students towards simulation based education.
All the students who participated in the studies and kindly shared your experiences and attitudes from participating in the simulations.
- Billings DM, Halstead JA (2005) Teaching in Nursing: A Guide for Faculty (2nd ed.). Philadelphia: W.B. Saunders.
- Alinier G (2007) A typology of educationally focused medical simulation tools. Medical Teacher 29: e243–e250 .
- Ryan CA, Walshe N, Gaffney R, Shanks A, Burgoyne L et al. (2010) Using standardized patients to assess communication skills in medical and nursing students. BMC Med Educ 10: 24 .
- Jeffries PR (2005) A framework for designing, implementing, and evaluating simulations used as teaching strategies in nursing. Nurs Educ Perspect 26: 96-103 .
- Rodgers DL (2007) High fidelity patient simulation: Descriptive white report, healthcare simulation strategies .
- The INASCL Board of Directors (2011) Standards of best practice: simulation. Clin Simul Nurs 7: S3-S19 .
- Gaba DM (2004) A brief history of mannequin-based simulation and application,” in Simulators in Critical Care and Beyond, WF Dunn, Ed, Society of Critical Care Medicine, Des Plaines, Ill, USA.
- Orledge J, Phillips WJ, Murray WB, Lerant A (2012) The use of simulation in healthcare: From systems issues, to team building, to task training, to education and high stakes examinations. Curr Opin Crit Care 18: 326-332 .
- Aebersold M, Tschannen D (2012) Using virtual simulations in second life for teaching and learning in nursing education. In R Hinrichs, C. Wankel (Eds.), engaging the avatar and transforming virtual world learning. Charlotte, NC: Information Age Publishing.
- Kyle RR, Murray WB (Eds.) (2008) Clinical Simulation: Operations, Engineering and Management. Burlington, MA: Academic Press .
- Pınar G, Dogan N (2013) Improving Perinatal Patient Safety Among Turkish Nursing Students Using, Simulation Traning Social and Behavioral Sciences 83: 88-93 .
- Sigalet E, Donnon T, Grant V (2012) Undergraduate Students’ Perceptions of and Attitudes Toward a Simulation-Based Interprofessional Curriculum. The KidSIM ATTITUDES Questionnaire. Simul Healthc 7: 353-358 .
- Ross AJ, Anderson JE, Kodate N, Thomas L, Thompson K, et al. (2013) Simulation training for improving the quality of care for older people: an independent evaluation of an innovative programme for inter-professional education. BMJ Qual Saf 22: 495–505 .
- Tawalbeh L, Tubaishat A. (2014) Effect of Simulation on Knowledge of Advanced Cardiac Life Support, Knowledge Retention, and Confidence of Nursing Students in Jordan. J Nurs Edu 53: 38-44 .
- Sammer CE, Lykens K, Singh KP, Mains DA, Lackan NA (2010) What is Patient Safety Culture? A Review of the Literature. J of Nurs Schol 42: 156-165 .
- Locsin RC, Purnell MJ (2013) Rapture and Suffering with Technology in Nursing. In WK Cody (Ed.), Philosophical and theoretical perspectives for advanced nursing practice 257-266.
- Botma Y (2014) Nursing student’s perceptions on how immersive simulation promotes theory–practice integration. International J of Afr Nurs Sciences 1: 1-5 .
- Dieckmann P, Friis SM, Lippert A, Ostergaard D (2012) Goals, Success Factors, and Barriers for Simulation-Based Learning A Qualitative Interview Study in Health Care. Simulation & Gaming 43: 627-647 .
- Ganley BJ, Linnard-Palmer L (2012) Academic Safety during Nursing Simulation: Perceptions of Nursing Students and Faculty. Clinical Simulation in Nursing 8: e49-e57 .
Article Alerts
Subscribe to our articles alerts and stay tuned.
 This work is licensed under a Creative Commons Attribution 4.0 International License.
This work is licensed under a Creative Commons Attribution 4.0 International License.

 Save to Mendeley
Save to Mendeley
