Archives of Nursing Practice and Care
Welcoming protocol in the maximum restriction of the emergency department of a tertiary hospital in Brazil
Juliane Martin Prestes1, Allant Silva Klein2, Alexandra Jochims Kruel2, Angelise Maria Martins1, Carolina Ritter Ribeiro3 and Fernando Anschau3,4*
2Hospital Nossa Senhora da Conceição (HNSC), Rio Grande do Sul, Brazil
3Graduation Program on Evaluation and Production of Technologies for the Brazilian National Health System, HNSC, Rio Grande do Sul, Brazil
4Health Technology Assessment Center (NATS), HNSC, Rio Grande do Sul, Brazil
Cite this as
Prestes JM, Klein AS, Kruel AJ, Martins AM, Anschau F, et al. (2020) Welcoming protocol in the maximum restriction of the emergency department of a tertiary hospital in Brazil. Arch Nurs Pract Care 6(1): 035-041. DOI: 10.17352/2581-4265.000047When we identify moments of extreme demand for health care in the Emergency Departments (ED), we can reach a level characterized as a maximum restriction, when there is an extreme decrease in the capacity to absorb new demand in the sector (capacity above the maximum number of beds arranged in the ED with hospital capacity preventing internal transfers). At these times, it is important to have alternatives to maintain health care for patients who seek emergency care.
This paper reports the description and validation of a nursing care protocol in an emergency department using a welcoming technique. In this technique, health production and promotion practices imply the responsibility of the health team for the user, from their arrival until the resolution of the illness that took them to the hospital.
Introduction
The maximum capacity of the Emergency Department (ED) occurs when the need for emergency services exceeds the availability of its resources. At this moment, we can characterize the work in the sector as a maximum restriction [1]. Overcrowding is a worldwide and multifaceted phenomenon. Its causes can be internal and external to the service, structural, and functional. Its consequences are harmful both to patients and health professionals, as well as to the services themselves, to the health care network, and, in a broader understanding, to society. For patients, the overcrowding of emergency services leads to increased waiting times for care and to obtain beds in units more appropriate for hospitalization, increased risk of adverse events, increased risk of worsening clinical conditions, autonomy loss, and mortality [2]. For health professionals, overcrowding creates work overload, culminating in stress, errors, accidents, and work-related illnesses. For the service, there is an increase in material costs and the need to expand the staff, which is sometimes replaced by overtime granting.
The moment of maximum restriction in ED is a complex issue caused by many extrinsic and intrinsic factors [1-4]. Despite the interaction between these causal factors, the consequence is the extreme decrease in the capacity to absorb new demand. However, according to the National Humanization Policy of Brazil (NHP), the patient has the right to welcoming, which presupposes “the change of the professional/user relationship and his/her social network through technical, ethical, humanitarian, and solidarity parameters, recognizing the user as a subject and active participant in the health production process” [5].
The welcoming would be a constitutive process of the practices of production and health promotion that implies the responsibility of the worker/team by the user, from his/her admission until his/her discharge. Listening to his/her complaint, considering his/her concerns and anxieties, using qualified listening that makes it possible to analyze the demand and, placing the necessary limits, guaranteeing comprehensive, resolutive, and responsible attention through the activation/articulation of the internal networks of services (aiming at horizontal care) and external networks, with other health services, for continuity of assistance when necessary [5-8].
Here, we identified a great similarity between the concepts of welcoming as a qualification strategy and lean thinking in health. From the Toyota production system, lean when applied to health is understood as a means to provide changes in the organization and hospital management, improving the quality of patient care and reducing errors and waiting times, besides benefiting the departments’ joint functioning of the departments [9]. Because it is a change of culture and not just the application of tools, successful implementation of lean goes through, in addition to training, pilot project, and implementation of improvements through assistance teams.
In this sense, the welcoming demands an organization of the work processes, aiming to serve those who seek health services, listening to their requests, assuming a posture of listening and agreeing on appropriate responses, providing care with resolution and responsibility, “guiding, when if applicable, the patient and family in relation to other health services for the continuity of assistance and establishing links with these services to ensure the effectiveness of these referrals” [5].
The present study demonstrates the elaboration, implementation, and the first results of the “Welcoming Protocol in the Maximum Restriction of the Emergency Department” by the nursing team.
Methodology
The nursing team carried out a descriptive study of the elaboration, validation, and implementation of a protocol at the ED of Hospital Nossa Senhora da Conceição (HNSC). These protocol creation processes, identified as “Welcoming Protocol in the Maximum Restriction of the Emergency Department”, followed some Lean healthcare guidelines and the application of validation instruments by a panel of experts [9,10]. The results of the pilot study of its use have also been described. The GHC Research Ethics Committee approved the study (protocol REC/GHC no. 3.730.887/CAAE 24851219.2.0000.5530) within this scope of measurement of care qualification.
The creation and implementation of a welcoming tool in situations of overcrowding
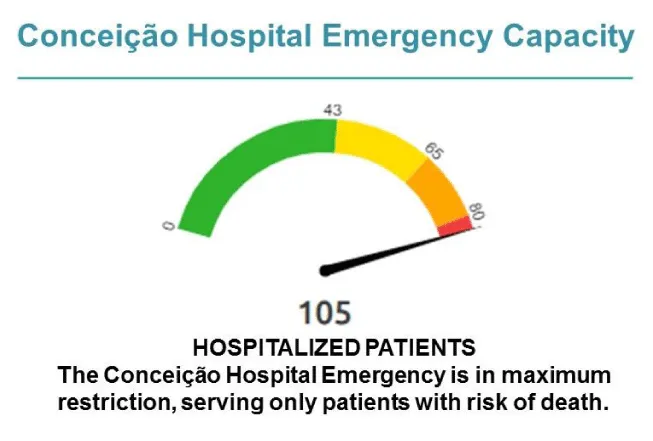
Faced with situations of extreme capacity of the ED, the Hospital Nossa Senhora da Conceição (HNSC) adopted the so-called Full Capacity Plan. This contingency plan provides for the maximum restriction of services when the number of patients in care in the ED exceeds the capacity installed. The hospital’s capacity does not allow the relocation of patients. Monitoring the ED capacity takes place daily and is shown on a panel on the HNSC website, as shown in Figure 1.
However, the restriction measure needs to be based on welcoming and safety for patients and professionals. To this end, in December 2018, the HNSC started working on a way to better guide people who seek their emergency in times of overcrowding (maximum restriction). Such an action would be carried out before the risk classification, aiming to offer welcoming with good guidance and safety to patients and professionals.
In this way, an instrument was created with the definition of clinical criteria to provide security to the professionals who would receive the patients. It is a checklist form, including two groups of questions to be answered with yes or no.
The first group of questions refers to how the patient is referred to the service and/or linked to the hospital:
• Regulated by the Mobile Emergency Care Service (MECS)?
• Previous acceptance of the Internal Regulation Nucleus (IRN)?
• In cancer follow-up at the hospital?
• Surgery performed at this hospital with a complaint related to the procedure?
• Referred from the Outpatient Clinic through contact with the ED’s duty?
The second group of questions refers to certain clinical changes to be observed:
• Behavior change?
• Precordial pain?
• Ventilatory suffering?
• Seizure in activity or post-ictal?
• Change of conscience?
• Intense visible bleeding?
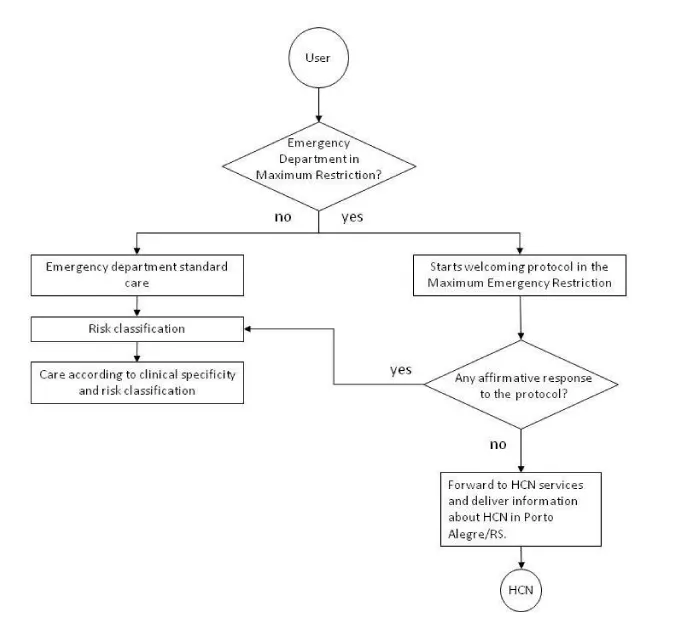
If there is at least one affirmative response, in any of the groups of questions, the patient moves to the risk classification stage. In case all responses are negative in both groups, the patient is referred to the services of the Health Care Network (HCN) and receives written information about the HCN in Porto Alegre/RS (Figure 2).
The definition of the items for the welcoming checklist in the maximum emergency restriction
The criteria to create the Welcoming checklist in the Maximum Emergency Restriction were defined considering situations that represent immediate risk or potential risk of life since no similar instrument was found in the literature to meet the need to restrict the care of the Adult Emergency of HNSC. Still, they consider the resources that the institution can provide, absorbing patients who need tertiary treatment and referring patients who can be seen in the Basic Health Network, in Emergency Care Units (ECU), or secondary hospitals.
Regarding the criteria for referred patients
Regulated by MECS: MECS assists emergency calls at home and in urban areas - on public roads - directing patients to the most appropriate health care ED institution, as established by the SUS National Regulatory Policy [11]. In this way, pre-hospital screening of patients is carried out, referring cases with already evidenced severity classification to the hospital’s ED.
Prior acceptance of the IRN: One of the functions of the HNSC’s IRN is the analysis of requests for assessments/hospitalizations of critically ill patients via emergency, coming from less complex institutions such as, for example, the ECU. Therefore, every patient assessed and considered serious by the IRN must be seen even during a period of maximum restriction in the ED.
Cancer follow-up at the hospital: Cancer patients are potentially immunosuppressed, both due to aspects related to the disease and to the therapies used in the treatment, being considered vulnerable to infections and rapid evolution to septic shock. Also, the national policy for the prevention and control of cancer in the health care network of people with chronic diseases within the scope of SUS establishes emergency care for cancer patients in hospitals, ensuring comprehensive care within the health care network [12]. Thus, all patients undergoing cancer follow-up at HNSC must be seen at the ED, even during maximum restriction periods. Still, the emergency of HNSC has the Febrile Neutropenia Protocol, widely applied in these patients.
Postoperative of surgery performed in this hospital with complaints related to the procedure: Due to the specificities related to the various surgeries and the potential postoperative complications, with a likelihood of suture dehiscence, profuse bleeding, or the presence of phlogistic signs at the surgical site, these patients may need immediate drug treatment, urgent exams, and even surgical reintervention.
Referral from the Outpatient Clinic through contact with the ED duty: The HNSC outpatient clinic performs elective appointments; however, sometimes, they are faced with the worsening of their patients’ clinical condition, requiring urgent hospitalization. Furthermore, it may lack diagnostic resources more quickly, such as laboratory collections, CT scans, ultrasounds, neurological evaluations, etc. In these situations, the outpatient clinic doctor makes telephone contact with the ED on duty and justifies the need for urgent evaluation. Once accepted by the emergency duty doctor, the patient is promptly referred from the outpatient clinic to the ED.
Regarding the criteria for spontaneous demand
• Behavior change: Changes in behavior such as acute mental confusion, aphasia, deviation of the labial commissure, loss of strength in the upper or lower limbs, and severe headache are signs and symptoms compatible with the presence of stroke. The emergence of HNSC has a stroke protocol in place and is a reference for treating ischemic stroke. Therefore, the clinical diagnosis must be defined within the time for thrombolysis (up to 4 hours after the onset of symptoms). In the case of hemorrhagic stroke diagnosis, the patient must be transferred to the Cristo Redentor Hospital, a reference for this nosological entity, immediately.
Precordial pain: Precordial pain is the main symptom of acute myocardial infarction, a cardiac emergency. This pain can spread to the upper limbs, neck, and face, and be accompanied by symptoms such as nausea and vomiting, altered consciousness, and hypotension. The care must be immediate, with an electrocardiogram performed in the first 10 minutes of ED admission. Time is a fundamental factor for the benefit of treatment, both immediate and late [13].
Ventilatory distress: In ventilatory distress, the need for immediate ventilatory support is observed. Signs and symptoms such as low oxygen saturation, tachypnea, tachycardia, shallow breathing, and cyanosis are perceived. It can be caused by acute conditions such as pulmonary embolism, chest injury, stroke, myocardial infarction, and an abrupt worsening of chronic obstructive pulmonary diseases (COPD) such as pulmonary emphysema, asthma, and bronchitis. In this case, the patient is directly referred to the emergency room.
Seizure in activity or post-ictal: Patients who enter ED presenting tonic or clonic movements may be in active seizure and should receive immediate care, assessing the need for drug intervention and protecting the nervous system from damage. Also, patients who have undergone a seizure with spontaneous relief, but arrive at the emergency in a post-ictal state with a sensory reduction should be observed in the emergency department.
Altered consciousness: Situations such as hypoglycemia, hypotension, exogenous intoxication, sepsis, and stroke can present acute sensory reduction, evidenced by the Glasgow scale. In these cases, care at the ED is essential.
Intense Visible Hemorrhage: Situations involving bleeding, as in the postoperative period, major hematuria, upper or low digestive hemorrhage, and profuse vaginal bleeding, are potential risk factors for hypovolemic shock and should be treated promptly in ED. In cases where the hemorrhage is due to trauma, the case should be stabilized, and then, the patient should be transferred to the Cristo Redentor Hospital, a reference in trauma.
Instrument validation
The instrument, already organized and structured, was submitted to an expert panel in the emergency area, composed of eight nurses, so that its content could be assessed, and the result of this stage constituted a qualification to the initial object. Nurses were listed according to the following criteria: having participated in the emergency department’s assistance team for more than five years and having experience with formulating protocols or publications on the topic. All eight nurses were from Rio Grande do Sul, with academic training in the metropolitan region of the state capital, and previously consented to assess the instrument. The average time of training was 16.7 years, and the emergency care experience was 11.2 years. Five nurses had teaching experience. At this stage, aspects such as clarity, comprehensiveness, and relevance or representativeness were observed for the instrument as a whole and afterward for each item. The agreement of the expert panel members was verified quantitatively through the content validity index (CVI) and qualitatively, with the interaction between the researchers/developers of the instrument and the panel experts. The assessments were individual and, besides the experts’ scores on each item, the questionnaire was open to suggestions from the group.
The instrument was considered comprehensive, clear, and relevant; its items were considered adequate and representative of the desired construct. The CVI among the panel experts was 0.96, which shows good agreement of the items. Three items of the protocol received CVI: 0.87 (in cancer follow-up at the hospital; referral to the outpatient clinic through contact with ED and altered consciousness), still satisfactory. However, they were better explained in the qualitative analysis, along with the item surgery performed in this hospital with complaints related to the procedure. Among these items, they were better spelled out, and the final version of them already appears above in the description of each one. The item related to previous surgery at the institution initially brought a cut-off point in the time elapsed between surgery and the time of emergency care, which was removed at this stage of instrument validation.
Implementation
Facilitators have been identified as an implementation strategy used to build practical capacity and support changes in practice to improve health care outcomes. Regardless of the level of change, individual or institutional, four facilitation strategies to adapt contextual factors and support changing practices are effective: (a) flexibility to align with organizational practices and priorities; (b) building relationships; (c) valuation through experience in information technology; and (d) capacity development and efficiency generation [14].
At the HNSC, these four strategies were used to some degree to get to what we wanted at the beginning, the implementation of the welcoming protocol in the maximum restriction of the emergency.
Results - The HNSC experience
At HNSC, in January 2019, a pilot was conducted in two phases. The first occurred on 01/15/2019 (Tuesday), and the second, on 01/21/2019 (Monday), both from 9:00 am to 7:00 pm, which is the period of greatest demand for the service.
On 01/15/2019, a poster was installed at the ED door, communicating the reality of overcrowding and maximum restriction. Two security guards were deployed inside the lobby and were waiting for patients to knock on the door. In these cases, a nurse welcomed patients close to the entrance door and identified the presence of any of the criteria established for care. If so, the patient was referred to the Risk Classification (RC). If not, the patient was instructed to seek the Emergency Care Unit or another service and was given a pamphlet with their addresses. Patients arriving in cars/ambulances were assessed in the vehicle by a nurse, followed by a security guard.
On this first day, 123 people sought the Emergency. The outcomes were described in Table 1. After that date, the team of professionals met to assess what happened and considered the positive and negative aspects. As positive aspects, it was noticed: (a) greater physical protection for the nursing professional, who assesses the patient inside the lobby; (b) assessment close to the door facilitates referral to other services; (c) the security team is more available to control access to the service; (d) the security guard accompanies the nurse in vehicle assessment; (e) the external information (poster) obtained a satisfactory result, as 32.5% of users sought another service on their own.
On the other hand, it was understood that the professional’s permanence at the door did not always provide an adequate assessment; in times of greatest demand, there was a queue at the door, and the nurses worked without registering their assessment. From there, some changes were proposed for the second phase of the pilot.
On 01/21/2019, the patient entered, registered, and waited for the nursing welcoming in the ED lobby. According to the instrument already presented, the nurse welcomed the patient to the screening office and identified the presence of any of the criteria established for care to define which flow to follow (risk classification or guidance to seek another service). Also, the welcoming was registered in a white bulletin. That day, the emergency door demand was 181 admissions. The outcomes were described in Table 2.
It is worth mentioning that, besides the total number of patients who sought care, other 70 knocked on the ED’s door to request general information, such as scheduling tests, in addition to requesting the use of a bathroom and drinking fountain.
After that date, the team of professionals met again to assess what happened. As positive aspects, several points were perceived as: (a) more effective and humanized welcoming, with better acceptance of referral by the patient; (b) there was no queuing at the door as it was organized using the take-a-number system and inside the lobby; (c) security guards were available to control access to the service; (d) the security guard accompanies the nurse in vehicle assessments; (e) the external information (poster) obtained a satisfactory result since 47% of users sought another service on their own.
An important aspect to highlight is the fact that we can access the data from the emergency care network and emergency services to identify the correct path taken by the referred patients. However, identifying the outcome of patients who simply, after reading the poster, go to other services, is still a point of limitation in the implementation of the protocol and aspect listed as a proposal for future studies.
This “pilot” experience was followed by the emergency care service organization and the computerization of the protocol, as shown in Figure 2. In this phase, all those aspects listed as important and priority in the assessment/welcoming of patients made up the checklist, as well as a space for other observations that could be part of the patient’s assessment and be fundamental for decision making (observation field).
Following the principles of continuous improvement and respect for people, advocated by the lean culture of lean in health, spaces for discussion, and collective construction of improvements to the protocol were created [15].
We were able to observe that the welcoming protocol in the maximum emergency restriction acts as an object of qualification of the hospital door of urgency and emergency, besides organizing and qualifying the care when this situation is “maximum restriction”, thus collaborating with the Urgency Care Network and Emergencies [16]. The protocol contributes to the humanization of care, focusing on comprehensive care for the user.
Discussion
In this study, we adopted embracement as a strategy to review health promotion practices in high demand situations in an emergency department to, according to the risk classification, guarantee referenced access to other levels of care.
A systematic review studied causes, effects, and solutions of overcrowding in emergency departments, finding 4,271 studies, of which 93 were selected. Of these, 33 articles addressed causes, 27 articles studied effects, and 40 articles studied overcrowding solutions. Commonly studied causes for overcrowding included nonurgent visits, patients classified as “frequent passengers”, influenza season, care with unqualified staff, hospitalization, and lack of hospital beds. Commonly studied effects included patient mortality, transport delays, treatment delays, ambulance diversion, patient flight, and financial effects. The listed solutions included additional human resources, observation units, access to the hospital bed, nonurgent referrals, ambulance diversion, control of patients’ destination, overcrowding measures, and queuing theory. This study illustrates the complex characteristics of the ED overcrowding problem [2].
Another strategy available in the literature is the maximum capacity protocol that suggests that when a patient needs to be admitted to an inpatient unit from the ED and that unit cannot accommodate the patient due to the lack of available beds, he/she will be admitted to the next most appropriate bed. Although the impacts of this type of protocol on patients admitted to inpatient units have not been fully studied, they bring the possibility of decreasing the length of stay in ED, less waiting time, fewer patients leaving the ED unseen, less patient mortality, greater operating income, and greater patient satisfaction [3]. Despite these favorable points, this maximum capacity protocol would not be a feasible alternative for many hospitals, as there is still a lack of a standard definition of the maximum capacity protocol and implementation strategies, as well as an alternative to management when the inpatient units are overcrowded, at the same time as the ED (the one characterized with maximum restriction).
In this study, the moment of maximum restriction in the ED is a complex issue caused by many extrinsic and intrinsic factors, the consequence of which is the extreme decrease in the capacity to absorb new demand in the sector (capacity above the maximum number of beds arranged in the ED with hospital capacity preventing internal transfers). In hospital care, the aim was to implement reception mechanisms with welcoming to users and welcoming with risk classification in the areas of access to the environment (emergency care/emergency room, outpatient clinic, and SADTs). In turn, specifically in urgent and emergency services, the aim was “the demand received and met according to the risk classification, guaranteeing access referenced to other levels of assistance” [6]. Lean management is another quality assurance method that focuses on process improvement and change management. Reducing unnecessary delays in ED is the ultimate goal to assure better patient outcome. The lean approach, such as that proposed by the welcoming protocol, can improve the patient flow in ED [9]. Adequately welcoming users who arrive at the ED in times of maximum restriction is proposed as an objective in constructing a welcoming protocol.
As already identified in the literature, the adoption of nonurgent referral measures and control of the patients’ destination (adequate referral) are strategies that can assist in the management of ED overcrowding [1,2,7,8].
- Schneider SM, Gallery ME, Schafermeyer R, Zwemer FL (2003) Emergency department crowding: A point in time. Ann Emerg Med 42: 167–172. Link: https://bit.ly/3nl7jSW
- Hoot NR, Aronsky D (2008) Systematic Review of Emergency Department Crowding: Causes, Effects, and Solutions. Ann Emerg Med 52: 126-136. Link: https://bit.ly/3l3wV4E
- Alishahi Tabriz A, Birken SA, Shea CM, Fried BJ, Viccellio P (2019) What is full capacity protocol, and how is it implemented successfully? Implement Sci 14: 73. Link: https://bit.ly/2Gp23fY
- Durand AC, Gentile S, Devictor B, Palazzolo S, Vignally P, et al. (2011) ED patients: How nonurgent are they? Systematic review of the emergency medicine literature. Am J Emerg Med 29: 333-345. Link: https://bit.ly/3inH3DE
- Brasil (2010) Ministério da Saúde. Secretaria de Atenção à Saúde. Núcleo Técnico da Política Nacional de Humanização. Ministério da Saúde. PORTARIA GM/MS No 4.279, DE 30 DE DEZEMBRO DE 2010. Estabelece diretrizes para a organização da Rede de Atenção à Saúde no âmbito do Sistema Único de Saúde (SUS). Brasília. 72.
- Brasil (2009) Ministério da Saúde. Secretaria de Atenção à Saúde. Política Nacional de Humanização da Atenção e Gestão, SUS D. PNH - Acolhimento e classificação de risco nos serviços de urgência. Ministério da Saúde. Secretaria de Atenção à Saúde. Política Nacional de Humanização da Atenção e Gestão do SUS 56.
- Dogherty EJ, Harrison MB, Baker C, Graham ID (2012) Following a natural experiment of guideline adaptation and early implementation: A mixed-methods study of facilitation. Implement Sci 7: 9. Link: https://bit.ly/3laEVRh
- Dogherty EJ, Harrison MB, Graham ID, Vandyk AD, Keeping-Burke L (2013) Turning knowledge into action at the point-of-care: The collective experience of nurses facilitating the implementation of evidence-based practice. Worldviews Evidence-Based Nurs 10: 129-139. Link: https://bit.ly/3cTSnq6
- Chan HY, Lo SM, Lee LLY, Lo WYL, Yu WC, et al. (2014) Lean techniques for the improvement of patients’ flow in emergency department. World J Emerg Med 5: 24-28. Link: https://bit.ly/36pRAvJ
- Hyrkäs K, Appelqvist-Schmidlechner K, Oksa L (2003) Validating an instrument for clinical supervision using an expert panel. Int J Nurs Stud 40: 619-625. Link: https://bit.ly/30qNqQw
- Brasil (2008) Ministério da Saúde. Secretaria de Atenção à Saúde. PORTARIA No 1.559, DE 1o DE AGOSTO DE 2008 Institui a Política Nacional de Regulação do Sistema Único de Saúde - SUS. Diário Of da União 1-5.
- Brasil (2013) Ministério da Saúde. Secretaria de Atenção à Saúde. PORTARIA No 874, DE 16 DE MAIO DE 2013 Institui a Política Nacional para a Prevenção e Controle do Câncer na Rede de Atenção à Saúde das Pessoas com Doenças Crônicas no âmbito do Sistema Único de Saúde (SUS). Diário Of da União 1–12.
- Avezum Junior Á, Feldman A, Carvalho ACDC, Sousa ACS, Mansur ADP, et al. (2015) V Diretriz da Sociedade Brasileira de Cardiologia sobre Tratamento do Infarto Agudo do Miocárdio com Supradesnível do Segmento ST. Arq Bras Cardiol 105: 1-105.
- Nguyen AM, Cuthel A, Padgett DK, Niles P, Rogers E, et al. (2019) How Practice Facilitation Strategies Differ by Practice Context. J Gen Intern Med [Internet] 35: 824-831. Link: https://bit.ly/30qNgIC
- Rees GH, Gauld R (2017) Can lean contribute to work intensification in healthcare. J Heal Organ Manag 3: 369-384. Link: https://bit.ly/3ioEssY
- Brasil (2013) Ministério da Saúde. Secretaria de Atenção à Saúde. Departamento de Atenção Especializada. Manual Instrutivo da Rede de Atenção às Urgências e Emergências no Sistema Único de Saúde (SUS) [Internet]. 1st ed. Brasília: Editora do Ministério da Saúde 86. Link: https://bit.ly/2HP5RrE

Article Alerts
Subscribe to our articles alerts and stay tuned.
 This work is licensed under a Creative Commons Attribution 4.0 International License.
This work is licensed under a Creative Commons Attribution 4.0 International License.
 Save to Mendeley
Save to Mendeley
