Archives of Nursing Practice and Care
Psychological wellbeing and mental health outcomes in Australian Nurses and Midwives
Louise Gibson and Kimberley Norris*
Cite this as
Gibson L, Norris K (2022) Psychological wellbeing and mental health outcomes in Australian Nurses and Midwives. Arch Nurs Pract Care 8(1): 017-027. DOI: 10.17352/2581-4265.000061Copyright License
©2022 Gibson L, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.Aim: To examine the intrapersonal and organizational factors that contribute to pathogenic and salutogenic psychological outcomes in Australian nurses and midwives.
Design: The conceptual framework Factors associated with Salutogenic and Pathogenic Outcomes in Australian Midwives and Nurses was used as a guide for this exploratory, cross-sectional study.
Method: Participants were recruited from public, private, and community settings throughout Australia. Six hundred and fifteen participants completed an online survey assessing job satisfaction, professional quality of life, ways of coping, resilience, psychological distress, and the impact of the worldwide coronavirus pandemic on psychological health and well-being.
Results: Analyses showed that workplace environmental factors were strong predictors of Secondary Traumatic Stress, and Burnout. Results also showed that workplace factors and adaptive coping were predictive of the salutogenic outcomes of compassion satisfaction and resilience.
Conclusion: Adopting a salutogenic approach, focused on maximizing individual and organizational contributors to psychological health and wellbeing, provides a new way for organizations to develop strategies to decrease adverse psychological outcomes, promote well-being and better equip nurses and midwives to cope with the challenges of the healthcare environment.
Impact: The findings will be of interest to Chief Nurses, Midwifery Officers, healthcare organizations, and universities to target workplace, individual and interpersonal factors that promote health and wellbeing amongst nurses and midwives.
Introduction
Workplace stress has been identified as a key antecedent of nursing and midwifery attrition [1]. Researchers have found that fatigue, burnout, secondary traumatic stress, depression, and anxiety are more prevalent amongst nurses and midwives in comparison to other healthcare professionals [2]. Figley [3] identified nurses increased vulnerability to the negative work-related outcome of compassion fatigue due to the core nursing values of compassion and empathy. Compassion Fatigue (CF) is an accumulative psychological, physical, and spiritual exhaustion that can occur in those responsible for caring for other people [4]. Burnout (BO) and Secondary Traumatic Stress (STS) are two independent components of CF (Stamm, 2009) [5]. Burnout can develop in nurses and midwives from feelings of frustration when patient care is compromised, whereas STS can manifest from a sense of guilt from not being able to do more to rescue someone from hurt [6]. Evidence has shown that not all nurses and midwives suffer from BO or STS despite exposure to similar work-related stressors [7]. Instead, Compassion Satisfaction (CS) provides some nurses with a way of coping with the emotional demands of the 'cost of caring' [5].
Background
Compassion is a core value of nursing and midwifery and provides motivation to alleviate the pain and suffering of others [8]. The emotional demands of nursing work, including exposure to grief and adverse outcomes, and the challenges of the healthcare environment can make it difficult to align these values with patient care [9]. Nurses and midwives with CF experience dread, avoidance, and exhaustion when caring for patients [10] as well as anxiety, depression, detachment, pain, and a loss of interest in caring behaviors [11]. Social support networks are crucial for nurses and midwives to cope with the complex demands of patient care [12]. Social support facilitates adaptive coping behaviors through positive communication [13], a supportive management team [14], mentor-mentee relationships (Drury, et al. 2014), modeling compassionate care and creating a team culture [2]. As such, social support is a consistent negative predictor of CF [15] and a protective factor against adverse psychological outcomes [12].
Burnout Syndrome (BO) is the physical and emotional exhaustion from prolonged exposure to workplace demands [4]. BO is distinguished from CF in that it impacts people working in a variety of demanding roles, not just those who care for others. BO comprises three core dimensions: exhaustion (i.e., low energy, fatigue), cynicism (i.e., detachment, irritability, negative attitude towards patient care), and inefficiency (i.e., maladaptive coping, decreased productivity) [16]. Consequently, safety standards and patient care may be compromised [2]. Recent studies show that nurses and midwives working in Australia and overseas have moderate to high levels of BO [17]. Several studies have found that Australian midwives who report an unsatisfactory work-life balance are more likely to suffer from BO [18] due to heavy workloads, high attrition, budget constraints, and an aging workforce [19].
Secondary Traumatic Stress (STS) is the second component of CF. Figley [4] described STS as the distress experienced from exposure to other people’s trauma in the helping/healthcare professional context. The symptoms of STS resemble those caused by PTSD and include intrusive thoughts, re-experiencing events, and avoidance behaviors [19] along with fear, hopelessness, guilt, anger, and hypervigilance [20]. Nurses and midwives are at high risk for STS due to frequent exposure to the pain and suffering of others [21] and the empathetic relationship they have with patients [15].
Cognitive dissonance (or moral distress) is a significant predictor of STS (Craige, et al. 2016) and occurs when an individual’s behavior is inconsistent with their attitudes and beliefs [22]. Nurses and midwives can feel dissatisfied and experience dissonance when clinical practice is incompatible with their values, attitudes, and expectations [23]. Most recently, the coronavirus pandemic has drawn worldwide attention to the moral distress and ethical dilemmas that affect nurses and midwives [24]. Concerns about inadequate staffing, limited antibody testing, stigmatization and the allocation of scarce resources have negatively impacted psychological well-being [25].
CS depicts the sense of accomplishment that a nurse or midwife gains from providing optimal patient care and fulfilling their professional role [10]. CS aligns the negative experiences of caring for others with the salutogenic factors elicited from helping behaviors [4]. Work environments that promote CS amongst nurses and midwives consequently decrease the incidence of CF [26]. Research consistently shows that peer social support positively predicts CS and reduces CF [27]. Transformational leaders in the organization further encourage a supportive work culture and enhance CS amongst staff by providing clear goals of care, professional support, education, and recognition [26].
Resilience has been described as an individual's capacity to effectively adjust to stress or trauma [28]. In nursing and midwifery, this multifaceted construct is reliant on the quality of the work environment and an individual's ability to adapt to adversity [13]. External factors that impede resilience include work-role overload, poor interpersonal communication, time restraints, inability to provide quality patient care, inadequate social support, and limited recognition of skills and achievements [13]. Resilience in the workplace is enhanced when nurses experience autonomy and reward from their work [13]. Intrapersonal factors, including adaptive coping strategies, cognitive flexibility, and personal meaning, influence whether an individual can successfully recover from problems or obstacles [7]. High resilience amongst nurses and midwives increases job satisfaction, psychological well-being, interpersonal relationships, and professional quality of life [29]. Conversely, nurses with low resilience are more susceptible to psychological distress, including CF, BO, and STS [30].
Research on stress and coping in the workplace has identified that adaptive coping strategies (i.e., problem-focused coping, reappraisal, accepting responsibility) can relieve the adverse psychological effects that lead to CF, STS, and BO [31]. A substantial body of research identifies that problem-focused coping facilitates adaptive behavior by improving the person-environment relationship [32]. For example, a cross-sectional study of nurses, physicians, and care attendants working in various pediatric intensive care units in Spain found that coping styles were predictive of BO and PTSD amongst staff members [33]. Active coping strategies, such as problem-focused coping, resulted in less psychological distress than passive styles such as rumination and avoidance [33].
Research about CF, BO, and STS in nursing and midwifery has almost exclusively been understood using a pathogenic framework [34]. Applying Antonovsky's [35] theory of salutogenesis reframes the current focus on pathogenic outcomes in nursing and midwifery to the pursuit of wellness. Few studies have applied salutogenic theory to identify key contributors in nursing and midwifery. One rare exception, Stock’s [34] mixed-method, exploratory, the descriptive study suggested that the salutogenic qualities of passion, adaptive coping strategies, social support, and educational attainment are protective factors against the negative consequences of BO in nursing populations. The coronavirus pandemic has highlighted the vital role of nurses and midwives in our community. Despite this, there remains a paucity of evidence identifying intrapersonal and workplace factors that contribute to salutogenesis amongst Australian nurses and midwives. This is the first quantitative study to examine multiple variables and apply salutogenic theory to a large sample of Australian nurses and midwives employed nationally in different care settings, and in doing so provide insights into targets for intervention.
The study
The study aimed to examine the intrapersonal and organizational factors that contribute to pathogenic and salutogenic psychological outcomes in Australian nurses and midwives.
Hypothesis 1: Maladaptive coping strategies (avoidance, emotional distancing, confrontation) and negative workplace environment factors (heavy workload, conflict with colleagues, compromised patient care) would positively contribute to psychological distress (Compassion Fatigue, Secondary Traumatic Stress, and burnout), among Australian nurses and midwives whilst adaptive coping strategies and positive workplace environment factors would negatively contribute to psychological distress.
Hypothesis 2: Adaptive coping strategies problem-focused coping, social support, positive reappraisal) and positive workplace environment factors (performance rewards, peer social support, satisfaction with patient care provided) would positively contribute to salutogenesis (compassion satisfaction, work satisfaction, and resilience) amongst Australian nurses and midwives whilst maladaptive coping strategies and a negative workplace environment would negatively contribute to salutogenesis.
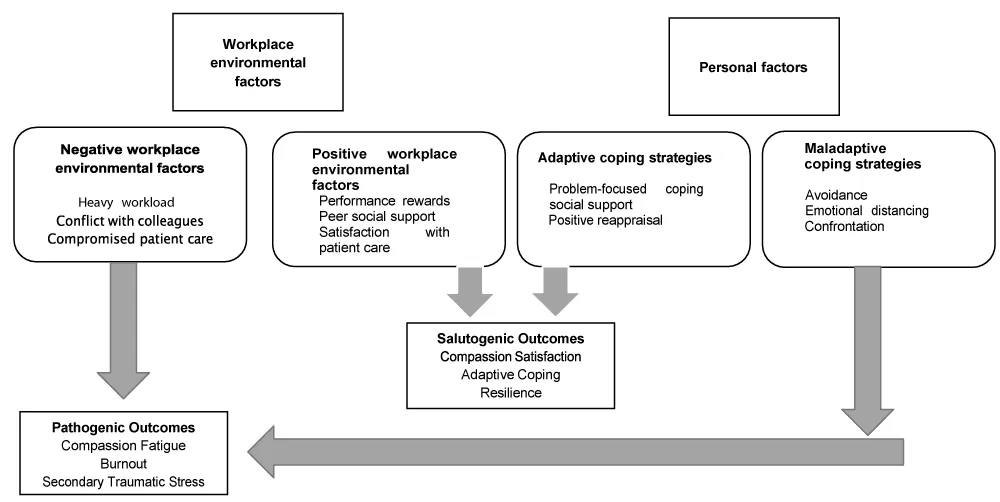
The researchers developed the Conceptual Framework, ‘Factors associated with Salutogenic and Pathogenic Outcomes in Australian Midwives and Nurses,’ for the study (Figure 1).
The framework depicts the personal and workplace environmental factors that determine pathogenic or salutogenic outcomes amongst this population.
Sample/participants
A convenience sample of 615 nurses and midwives was recruited from the public, private, and community settings from the 24th of May to the 24th of September 2020. The Tasmanian Social Sciences Human Research Ethics Committee approved the study (H0017396).
Materials/Measures
The assessment battery included the following measures:
Sociodemographic variables: Information about age, sex, and education were collected from participants.
Ways of Coping Questionnaire [36]: The revised WCQ is a 66-item self-report questionnaire that was used to determine the coping processes used by nurses and midwives in the current study. Eight different subscales were assessed: confrontative coping; distancing; self-control; seeking social support; accepting responsibility; escape-avoidance; planful problem-solving; and positive reappraisal [36]. Responses were measured using a 4-point Likert scale, ranging from 0 (not used) to 3 (used a great deal). Higher scores showed that this coping mechanism was used to a greater degree (i.e., low ≤66; moderate 67 - ≤132; high 133 - ≤198 WCQ)
Job Satisfaction Scale [37]: The JSS was used to determine job satisfaction amongst nurses and midwives. The 36-item self-report measure is comprised of a 6-point Likert scale ranging from 1 (disagree very much) to 6 (agree very much). The survey was used to assess employee attitudes in nine areas of job satisfaction: salary, promotion opportunities, supervision, fringe benefits, performance rewards, policies and protocols, co-worker relations, type of work, and communication. Scores of ≥ 4 were interpreted as satisfaction, whereas ≤ 3 suggest dissatisfaction. Scores between 3-4 represent job ambivalence.
Connor-Davidson Resilience Scale [38]: The 25-item CD-RISC was used to measure the resilience of nurses and midwives. Nurses and midwives reported how they felt over the past 30 days on a 5-point Likert scale ranging from 0 (not true at all) to 4 (true nearly all the time). Higher scores indicated a greater level of resilience.
Patient Health Questionnaire 4 [39]: The PHQ-4 is a brief 4-item screening tool that asked midwives and nurses about their mental health over the last two weeks. The scale identified depression and anxiety on a 4-point Likert scale ranging from 0 (not at all) to 3 (nearly every day). Psychological distress was measured as none (0-2), mild (3-5), moderate (6-8), and severe (9-12). Possible scores for anxiety and depression ranged from 0-6 and a score of ≥3 suggested clinically relevant depression or anxiety.
Professional Quality of Life Scale [5]; The ProQOL 30-item self-report scale was used to determine compassion satisfaction, compassion fatigue, burnout, and secondary traumatic stress amongst nurses and midwives. Items are scored on a 5-point Likert scale ranging from 1 (never) to 5 (very often). Scores were calculated on each subscale (compassion satisfaction, burnout, secondary traumatic stress) to show low (<43), average (43-57), or high (>57) levels of each construct.
COVID-19 Impact Scale; The research team designed a 15-item scale to determine the impact of the COVID-19 Pandemic. Participants were asked to respond using a 5-point Likert scale ranging from 1 (never) to 5 (all of the time). The questions asked participants to respond how strongly they agreed with each statement. A total score of 75 was possible, with higher scores suggesting a higher level of impact from the COVID-19 pandemic (i.e., low ≤25; moderate 26-≤50; high 51-75).
Results/Findings
Sample characteristics
The study participants ranged in age from 21 -74 years (Mage = 45 years, SD = 12.4). The sociodemographic characteristics of the participants are described in Table 1.
Descriptive statistics
Descriptive statistics are presented in Table 2. Results showed that Australian nurses and midwives are experiencing low levels of CS (score < 23), BO (score<23), STS (score<43); ambivalent job satisfaction (score 108-144), and moderate psychological distress (score 6-8) in the current healthcare climate.
Forced multiple regression statistical analysis and interpretation
Secondary traumatic stress: The model was a significant predictor of STS amongst Australian nurses and midwives, F(13, 241) = 3.50, p = < .001, and accounted for 11 % of the variability in STS (Table 3). Pay and process were significant predictors of STS in the linear regression model.
Burnout: Multiple Regression analysis showed that the predictors included in the model (Table 4) significantly predicted BO amongst Australian nurses and midwives, F(10,254) = 2.59, p = .005, and accounted for 6% of the variability of BO in this population.
Compassion satisfaction: The multiple regression model was a significant predictor of Compassion Satisfaction, F(7, 265) = 3.63, p = <.001, and explained 6% of the variance in the salutogenic construct (Table 5).
Resilience: The multiple regression model was a significant predictor for Resilience, F(10, 254) = 2.59, p = .005, and explained 6% of the variance of this construct (Table 6). Distancing, social support, nature of work, and anxiety were significant predictors of resilience.
Job satisfaction: The multiple regression model was a significant predictor for Job Satisfaction, F(5, 268) = 5.93, p < .001, explaining 10%of the variance in this construct (Table 7). The model indicated that depression was a negative predictor of JSS, whereas the coping strategy of control was a positive predictor.
Discussion
Australian nurses and midwives are experiencing low levels of CS, BO, and STS and ambivalent job satisfaction in the current healthcare climate. Consistent with previous research findings [29] resilience was shown to be high amongst Australian nurses and midwives, with scores in this sample aligning with the top 25 % of the general population. This demonstrates that salutogenic and pathogenic outcomes can occur independently, rather than on a continuum. Therefore, we need to identify the distinct contributors of each to maximize salutogenic and minimize pathogenic outcomes.
Australian nurses and midwives reported low levels of STS despite the reported moral distress, fear, and daily ethical concerns of nurses and midwives working throughout the coronavirus pandemic [21]. Our data were obtained from a diverse range of nurses and midwives employed nationwide who had varying experiences of COVID-19 and organizational systems which may explain the unexpected outcome of low STS in our sample.
CS was found to be low in this sample. Previous research examining the incidence of CS in nurses and midwives has found low- moderate levels [40]. Differences between the current and previous research may be that CS is influenced by workplace environmental factors. For example, intensive care nurses are exposed to frequent adverse outcomes, whereas mental-health nurses cope with greater levels of verbal/physical consumer aggression [41]. Concomitant with moderate levels of psychological distress findings suggest that Australian nurses and midwives are not experiencing high levels of motivation, nor a strong sense of purpose or reward for their work in helping others. This finding is supported by JSS results that showed ambivalence towards job satisfaction. It is thus suggested that some Australian nurses and midwives are experiencing reduced psychological health and well-being in their current work environments.
The hypothesis positing that maladaptive coping strategies and negative workplace environmental factors would positively contribute to psychological distress was partially supported. Although there was limited support for the influence of maladaptive coping strategies on pathogenic outcomes, negative workplace environmental factors contributed to pathogenic outcomes in the study. Pay and process (i.e., organizational rules, policies, and procedures) were the strongest negative contributors to STS in our model, whilst pay alone was the strongest negative contributor to BO in this population.
The second hypothesis, that adaptive coping strategies and positive workplace environmental factors would positively contribute to salutogenesis, was supported. The organizational process was negatively associated with CS, whereas the nature of work was positively associated with resilience. The adaptive coping strategies of distancing and social support seeking were negatively associated with resilience amongst the sample population. Finally, self-control was a coping mechanism identified as being positively associated with job satisfaction in Australian nurses and midwives.
Workplace environmental factors contributed to pathogenic and salutogenic outcomes in the current study. As expected, pay and operational processes were strong negative predictors of pathogenic outcomes. In contrast, the nature of work was a strong positive predictor of salutogenic outcomes. Consistent with previous research, these results suggest that Australian nurses and midwives feel that their pay scale is not commensurate with their qualifications and the work they do [42]. An international study by McVicar and colleagues (2003) recognized that discontent from low remuneration was becoming a more prominent source of job dissatisfaction in nursing, with Preston [43] reporting that 49.4% of Australian nurses were dissatisfied with their salary. A disparity between nursing/midwifery wages and education level has been widely reported in the literature [44]. Nursing salaries remain low relative to their professional counterparts [43]. Over half (57.3%) of the nurses and midwives in our sample held postgraduate qualifications which may exacerbate the seeming disparity between education and pay scale.
Our results are also consistent with those of Foster and colleagues [29] who suggested that organizational processes (i.e., workload, paperwork, procedures, policies) were strong negative contributors to pathogenic outcomes in Australian nurses and midwives. Foster, et al. [29] showed that inadequate staff-patient ratios and inexperience prompted distress amongst Australian mental health nurses in their study. The current research found organizational processes to be specific negative contributors to STS in Australian nurses and midwives. These findings are consistent with recent studies examining the impact of COVID-19 on nurses globally [45]. Maben, et al. [26] found that organizational processes, including staff shortages, long-shift hours, limited antigen testing procedures for staff, and insufficient personal protection equipment rendered staff exhausted and unable to provide patients with the usual standard of care.
Contrary to expectations, our results did not identify maladaptive coping as a contributor to psychological distress and pathogenesis. Past research has shown that maladaptive coping contributes to pathogenic outcomes in nurses and midwives [46]. The difference between expected and obtained results may be the very high resilience levels reported by nurses and midwives in our study. Nurses and midwives who participated in our study demonstrated three critical factors associated with resilience: increased age (Mage = 47 years), a high level of education (57.3% held postgraduate qualifications), and extensive professional experience (M = 20 years).
Several studies have demonstrated that adopting a passive coping style (i.e., distancing) to cope with stressful workplace environments can increase psychological distress [33]. The current findings support this argument, showing moderate levels of psychological distress amongst Australian nurses and midwives, suggesting that Australian nurses and midwives were at increased risk for these mental health conditions. Chang, et al. (2006) demonstrated similar observations in a study of Australian acute care nurses showing that distancing increased the incidence of adverse mental health. Evidence suggests that relying on distancing as a coping strategy can eventually lead to depersonalization, a predominant symptom of BO [4]. Education about adaptive coping strategies (i.e., problem-focused coping, seeking adequate social support) is one way that organizations can protect staff from CF, BO, and STS and sustain the provision of quality care over the long term [13].
Organizational processes (i.e., workload, paperwork, procedures, policies) were found to be negative contributors to CS in our study. Structural empowerment supports nurses and midwives to provide compassionate care by resourcing them with safe patient-care ratios, time, equipment, education, and organizational support [47]. Nurses and midwives are better able to provide compassionate care to patients when there is congruence with their personal, professional, and organizational values [48].
As expected, the nature of work (i.e., I feel a sense of pride in my job) positively contributed to resilience. This was consistent with the research [49] recognizing that personal meaning provides intrinsic motivation and protection against adverse psychological outcomes in healthcare workers. These results also reflect those of Galuska and Bursch [50] who showed that joy and meaning were essential for the overall well-being of a sample of American critical care nurses. Facilitating resilience in the workplace not only protects nurses from distress but improves their consideration towards others and adaptability to future unexpected events (Foster., 2018). Organizations must therefore support nurses and midwives to make connections between their daily work, personal meaning, values, and identity [50].
Chang [51] recognized that social support was one of the most common coping strategies used to foster resilience in a study of Australian and New Zealand nurses. Garnering social support is an active way that nurses and midwives can overcome adversity and stimulate positive feelings [52]. Our study differed from previous findings in that social support was identified as negatively contributing to resilience. Social support indicates obtaining informational, practical, and emotional care [53]. It is possible, therefore, that the social support from work colleagues and management currently received by Australian nurses and midwives is inadequate [54]. Previous research has claimed that Australian nurses and midwives are exhausted [55] and therefore may not be emotionally equipped to provide appropriate support to each other. Foster, et al. (2019) found that inadequate social support (i.e., condescending staff interactions, bullying, ineffective teamwork, laziness) was a major stressor in a sample of Australian mental health nurses. Comparatively, Harvie, et al. [56]. Recognized that prominent concerns, such as bullying, fear of blame, and unmanageable workloads, rendered Australian midwives feel unsupported. It can thus be suggested that our sample of nurses and midwives were not utilizing this coping strategy well, or that those around them were not able to provide appropriate social support due to the impacts of the work environment on their wellbeing.
Psychological distancing was also found to be a significant negative contributor to resilience amongst Australian nurses and midwives. Bussing, et al. [57], argued that although this coping strategy is common practice amongst nurses, it is not effective in the long term and has been associated with BO. Surprisingly, our study showed low BO in Australian nurses and midwives. A possible explanation for this might be that the symptoms of BO emerge gradually over time and may become apparent as the impacts of COVID-19 continue to emerge [57] or as an individual’s career progresses. In this way, distancing may be an effective short-term, but not long-term, a method for managing the stressors inherent in nursing and midwifery work.
Unsurprisingly, anxiety was a strong negative contributor to resilience in this population. A likely explanation for this result may be that data was collected whilst participants were caring for patients during the COVID-19 Pandemic; resources were inadequate, and policies and protocols to protect their wellbeing was limited [46]. Although anxiety is an adaptive emotional response to increased stress, evidence suggests that this psychological distress can manifest into lasting adverse physical and mental health outcomes Consistent with previous research, self-control was shown to be a positive contributor to job satisfaction. In nursing, this coping strategy involves not sharing thoughts and feelings with co-workers [51]. A study of Australian and New Zealand nurses showed that self-control, along with problem-focused coping and social support, was heavily relied on to cope with workplace stress [51]. Despite this, self-control was argued to be associated with adverse mental health outcomes in the long term [51]. This result may once again indicate that nurses and midwives are experiencing cognitive dissonance in the current healthcare environment [23]. Rather than obtaining meaning from their work through the provision of optimal patient care and close relationships with colleagues, our results suggest that nurses and midwives are coping in complex environments by relying on self-control. Self-control, like distancing, is a way of coping that is incompatible with the core values of nursing practice and often leads to increased distress again suggesting that nurses and midwives may be adopting strategies that, whilst effective in the short-term, contribute to longer-term distress.
Findings suggest that leadership styles that consist of effective communication and address the specific workplace problems identified by staff are vital in promoting job satisfaction and resilience amongst staff (Marin & Garcia-Ramirez, 2005) [58]. According to preliminary observations, deficient healthcare management strategies have been exposed as the worldwide COVID- 19 pandemic has unfolded [46]. Criticisms of poor leadership have been evidenced by outbreaks in aged care in Australia (COVID-19 and residential aged care Australia, 2020). This combination of findings provides some support for the conceptual premise that positive workplace environmental factors contribute to salutogenesis, whereas negative factors increase the risk of pathogenic outcomes amongst Australian nurses and midwives. Social support, teamwork, and positive relationships must be prioritized by healthcare management to sustain nurses and midwives not just in times of crisis but to promote salutogenic outcomes throughout their careers [59].
The identification of factors contributing to salutogenic and pathogenic outcomes in nurses and midwives provides an avenue for the development of interventions to maximize psychological health and well-being in this group of healthcare workers. Based on the results of the current study, workplace strategies to enhance psychological health and well-being in the nursing and midwifery sector could include the introduction of flexible shift arrangements, manageable/safe staff-patient ratios, and increased remuneration for nurses and midwives [60].
The findings of this study provide important insights into the psychological distress and job dissatisfaction that nurses and midwives are experiencing, despite being held up as global heroes throughout the coronavirus pandemic crisis [61]. Notably, this public discourse of heroism detracts from the workplace environmental stressors that are associated with decreased compassion satisfaction and job satisfaction in this population [61]. Jones, et al. [48], argued that these resultant inconsistencies may manifest as cognitive dissonance and create adverse psychological outcomes (i.e., CF, STS, BO) amongst nurses and midwives in the long term [48].
Although our findings demonstrated low STS and BO, low CS and ambivalent job satisfaction were evident in our results. These results may not only suggest that Australian nurses and midwives are struggling to obtain personal meaning and reward from their role but could also possibly indicate that they are not kind, empathetic, and compassionate to themselves [62]. Nurses and midwives who lack self-compassion are self-critical, judge themselves harshly, and experience reduced distress tolerance [62]. Self-compassion is fundamental for the well-being of nurses and midwives, enabling them to show care and compassion towards the patients whom they care for [62]. Organizations can encourage self-compassion and promote self-care amongst staff by offering well-being programs, mindfulness training, and compassion literacy education [63]. Compassion literacy promotes awareness about how nurses and midwives can ensure that their own personal and professional values align to provide compassionate patient care [8]. Once nurses and midwives understand the importance of compassion literacy, they are better able to provide compassionate care to others and engage in self-care themselves [8]. In turn, compassion satisfaction results from patient care rather than compassion fatigue [64]. Beaumont and colleagues [62] recognized the merits of developing a compassionate mind to promote resilience, adaptive coping, and compassion satisfaction. Long-term benefits to organizations include improved patient care, decreased staff turnover, and reduced absenteeism [62].
Current findings may help nursing and midwifery leaders to understand the barriers to providing compassionate care in their organizations [63]. Creating an environment that enables nurses and midwives to engage in clinical practice following their values may reduce adverse pathogenic outcomes, such as CF and BO, promote resilience and facilitate adaptive coping [63]. Many workplace environments currently rely on automaticity (e.g., tick-boxes on care plans) and superficial tactics to recognize the work of staff. Such approaches contrast with recommendations made by Jones, et al. [48], that environments be ‘warmed up to ensure a genuine approach to nursing/midwifery care that can increase job satisfaction, organizational commitment, and occupational identity. For example, a culture of caring can be demonstrated by relieving senior staff of excessive paperwork and availing them of incidental mentoring with junior staff [65].
Social support (i.e., relatedness) has been identified as predictive of resilience in complex healthcare environments [34]. Previous research has shown that job satisfaction and compassionate care are hindered in workplaces that do not encourage supportive relationships, teamwork, and positive interactions between staff (Burridge, et al. 2015). More experienced staff need to feel valued and respected in the workplace, whereas early career professionals need to feel guided and reassured in their practice [42]. Competence and autonomy can be achieved through effective mentoring and role modeling in the workplace [66]. In nursing and midwifery mentoring dually recognizes the value of experienced senior staff and the importance of supporting early practitioners. Mentors can model clinical skills, work-life balance, teamwork, interdisciplinary collaboration, optimism, and self-care [66].
Another vital issue from these findings is the necessity to expand nursing and midwifery curricula to provide education about psychological distress, adaptive coping strategies, resilience, and self-care [67]. Studies have shown that the global attrition rate of nurses less than one year after graduation is between 17-50% [68]. Forewarning students about the pathogenic outcomes that may result from clinical practice provides students with the opportunity to engage in self-care and develop resilience early, to sustain them throughout their professional careers [62]. Teaching compassion literacy and emotional resilience to undergraduate nursing and midwifery students reaffirm the core values of nursing and better prepare students for the workplace [8]. These findings may also help educators promote understanding of the importance of establishing collegial networks for nursing/midwifery students to sustain them throughout their careers [13].
Future research is needed to determine the effectiveness of strategies to reduce the negative consequences of BO, STS, and psychological distress amongst Australian nurses and midwives. A greater focus on social support, role conflict, available resources, and education may provide insight into why the variance between variables was small in this study and guide further work. Research into the development of educational programs to promote salutogenesis in nursing/midwifery throughout undergraduate programs and in the workplace is essential. Finally, implementing strategies to facilitate the well-being of Australian nurses and midwives over the course of their careers is critical to preventing adverse psychological outcomes, reducing attrition rates, and providing a robust healthcare workforce.
Limitations
Data collection for this study occurred during the worldwide coronavirus pandemic and as such may not be representative of the experiences of Australians and nurses outside the COVID context. Although the sample was representative of nurses and midwives practicing nationwide, some organizations declined participation reporting survey fatigue during the pandemic. In addition, unlike the other psychometric assessment scales, COVID-19 data was collected using an unvalidated questionnaire developed based on clinical knowledge and the MERS-CoV staff questionnaire. Further to this, despite the online self-report questionnaires being a convenient method to collect data, it is recognized that such data collection methods can be subject to bias [69-71].
Conclusions
The coronavirus pandemic has commanded public attention worldwide on the vital role that nurses and midwives play in our communities. Some suggest that the emotional toll and adverse psychological outcomes of caring for others on the frontline of healthcare have finally gained recognition [58]. Governments and organizations can no longer ignore the well-being of nurses and midwives and must initiate change to protect, recruit and guarantee community members a healthy workforce in the future. Importantly, the underlying cognitive dissonance demonstrated through low compassion satisfaction, ambivalent job satisfaction, and increased psychological distress in our findings must be resolved so that nurses and midwives can realign patient care with their core values. Identifying contributors to CF, STS, and BO is the first step toward understanding what is required to protect nurses and midwives from the ‘cost of caring’ [5]. Only then can the strategies to promote salutogenesis be cultivated in modern-day health care.
- Hämmig O. Explaining burnout and the intention to leave the profession among health professionals - a cross-sectional study in a hospital setting in Switzerland. BMC Health Serv Res. 2018 Oct 19;18(1):785. doi: 10.1186/s12913-018-3556-1. PMID: 30340485; PMCID: PMC6194554.
- Kinman G, Leggetter S. Emotional Labour and Wellbeing: What Protects Nurses? Healthcare (Basel). 2016 Nov 30;4(4):89. doi: 10.3390/healthcare4040089. PMID: 27916880; PMCID: PMC5198131.
- Figley C. Traumatization and comfort: Close relationships may be hazardous to your health. [Keynote presentation]. Families and close relationships: Individuals in social interaction. Conference held at the Texas Tech University. Lubbock. March 1982.
- Figley C. Epilogue: the transmission of trauma. In Compassion Fatigue: Coping with Secondary Traumatic Stress Disorder in Those who Treat the Traumatized. Taylor & Francis Group. 1995; 249-254.
- Stamm B. The concise ProQOL manual (2nd.). Pocatello. ID: ProQOL. 2009.
- Cocker F, Joss N. Compassion Fatigue among Healthcare, Emergency and Community Service Workers: A Systematic Review. Int J Environ Res Public Health. 2016 Jun 22;13(6):618. doi: 10.3390/ijerph13060618. PMID: 27338436; PMCID: PMC4924075.
- Delgado C, Roche M, Fethney J, Foster K. Workplace resilience and emotional labour of Australian mental health nurses: Results of a national survey. Int J Ment Health Nurs. 2020 Feb;29(1):35-46. doi: 10.1111/inm.12598. Epub 2019 May 3. PMID: 31050127.
- Burridge LH, Winch S, Kay M, Henderson A. Building compassion literacy: Enabling care in primary health care nursing. Collegian. 2017;24(1):85-91. doi: 10.1016/j.colegn.2015.09.004. PMID: 29218966.
- Balinbin CBV, Balatbat KTR, Balayan ANB, Balcueva MIC, Balicat MGB, Balidoy TAS, Macindo JRB, Torres GCS. Occupational determinants of compassion satisfaction and compassion fatigue among Filipino registered nurses. J Clin Nurs. 2020 Mar;29(5-6):955-963. doi: 10.1111/jocn.15163. Epub 2020 Jan 13. PMID: 31887244.
- Ruiz-Fernández MD, Pérez-García E, Ortega-Galán ÁM. Quality of Life in Nursing Professionals: Burnout, Fatigue, and Compassion Satisfaction. Int J Environ Res Public Health. 2020 Feb 15;17(4):1253. doi: 10.3390/ijerph17041253. PMID: 32075252; PMCID: PMC7068555.
- Hemsirelerinde P, Tukenmislik C, Yorgunlugu E, Yorgunlugu E, Iliski M. Relationship between liking of children and Burnout, Compassion Fatigue, Occupational Satisfaction in Paediatric Nurses, Turkiye Klinikleri Hemsirelik. 2020; 12:30-36. https://doi.org/10.5536.nurses.2019-70084
- Drury V, Craigie M, Francis K, Aoun S, Hegney DG. Compassion satisfaction, compassion fatigue, anxiety, depression and stress in registered nurses in Australia: phase 2 results. J Nurs Manag. 2014 May;22(4):519-31. doi: 10.1111/jonm.12168. PMID: 24926496.
- Mcdonald G, Jackson D, Vickers MH, Wilkes L. Surviving workplace adversity: a qualitative study of nurses and midwives and their strategies to increase personal resilience. J Nurs Manag. 2016 Jan;24(1):123-31. doi: 10.1111/jonm.12293. Epub 2015 Apr 13. PMID: 25865519.
- O'Callaghan EL, Lam L, Cant R, Moss C. Compassion satisfaction and compassion fatigue in Australian emergency nurses: A descriptive cross-sectional study. Int Emerg Nurs. 2020 Jan;48:100785. doi: 10.1016/j.ienj.2019.06.008. Epub 2019 Jul 19. PMID: 31331839.
- Maslach C, Leiter MP. Understanding the burnout experience: recent research and its implications for psychiatry. World Psychiatry. 2016 Jun;15(2):103-11. doi: 10.1002/wps.20311. PMID: 27265691; PMCID: PMC4911781.
- Fenwick J, Lubomski A, Creedy DK, Sidebotham M. Personal, professional and workplace factors that contribute to burnout in Australian midwives. J Adv Nurs. 2018 Apr;74(4):852-863. doi: 10.1111/jan.13491. Epub 2017 Nov 27. PMID: 29105143.
- Cramer E, Hunter B. Relationships between working conditions and emotional wellbeing in midwives. Women Birth. 2019 Dec;32(6):521-532. doi: 10.1016/j.wombi.2018.11.010. Epub 2018 Dec 19. PMID: 30578019.
- Guo YF, Plummer V, Lam L, Wang Y, Cross W, Zhang JP. The effects of resilience and turnover intention on nurses' burnout: Findings from a comparative cross-sectional study. J Clin Nurs. 2019 Feb;28(3-4):499-508. doi: 10.1111/jocn.14637. Epub 2018 Sep 3. PMID: 30091259.
- Leinweber J, Creedy DK, Rowe H, Gamble J. A socioecological model of posttraumatic stress among Australian midwives. Midwifery. 2017 Feb;45:7-13. doi: 10.1016/j.midw.2016.12.001. Epub 2016 Dec 6. PMID: 27960122.
- Mottaghi S, Poursheikhali H, Shameli L. Empathy, compassion fatigue, guilt and secondary traumatic stress in nurses. Nurs Ethics. 2020 Mar;27(2):494-504. doi: 10.1177/0969733019851548. Epub 2019 Jul 8. PMID: 31284826.
- Li Z, Ge J, Yang M, Feng J, Qiao M, Jiang R, Bi J, Zhan G, Xu X, Wang L, Zhou Q, Zhou C, Pan Y, Liu S, Zhang H, Yang J, Zhu B, Hu Y, Hashimoto K, Jia Y, Wang H, Wang R, Liu C, Yang C. Vicarious traumatization in the general public, members, and non-members of medical teams aiding in COVID-19 control. Brain Behav Immun. 2020 Aug;88:916-919. doi: 10.1016/j.bbi.2020.03.007. Epub 2020 Mar 10. PMID: 32169498; PMCID: PMC7102670.
- Festinger L. A Theory of cognitive dissonance. Stanford University Press. 1957.
- de Vries JMA, Timmins F. Teaching psychology to nursing students-a discussion of the potential contribution of psychology towards building resilience to lapses in compassionate caring. Nurse Educ Pract. 2017 Sep;26:27-32. doi: 10.1016/j.nepr.2017.06.004. Epub 2017 Jun 17. PMID: 28648957.
- McClunie-Trust P. Potential impacts of COVID-19 pandemic, Kai Tiaki Nursing New Zealand. 2020; 26:20-21.
- Maben J, Bridges J. Covid-19: Supporting nurses' psychological and mental health. J Clin Nurs. 2020 Aug;29(15-16):2742-2750. doi: 10.1111/jocn.15307. Epub 2020 Jun 2. PMID: 32320509; PMCID: PMC7264545.
- Henson JS. When Compassion is Lost. Medsurg Nurs. 2017 Mar;26(2):139-42. PMID: 30304598.
- Bjanca, V., Balinbin, C., Balabat, K., Balayan, A., Balcueva, M., Balicat, M., Balidoy, T., Macindo, J. & Torres, G. (2019). Occupational determinants of compassion satisfaction and compassion fatigue among Filipino registered nurses, Journal of Clinical Nursing, 29, 955-963. https://doi.org/10.1111/jocn.1516
- Manomenidis G, Panagopoulou E, Montgomery A. Resilience in nursing: The role of internal and external factors. J Nurs Manag. 2019 Jan;27(1):172-178. doi: 10.1111/jonm.12662. Epub 2018 Jul 31. PMID: 30066352.
- Foster K, Roche M, Giandinoto JA, Furness T. Workplace stressors, psychological well-being, resilience, and caring behaviours of mental health nurses: A descriptive correlational study. Int J Ment Health Nurs. 2020 Feb;29(1):56-68. doi: 10.1111/inm.12610. Epub 2019 May 25. PMID: 31127973.
- Ang SY, Hemsworth D, Uthaman T, Ayre TC, Mordiffi SZ, Ang E, Lopez V. Understanding the influence of resilience on psychological outcomes - Comparing results from acute care nurses in Canada and Singapore. Appl Nurs Res. 2018 Oct;43:105-113. doi: 10.1016/j.apnr.2018.07.007. Epub 2018 Jul 26. PMID: 30220356.
- Ames M, Salmond E, Holly C, Kamienski M. Strategies that reduce compassion fatigue and increase compassion satisfaction in nurses: a systematic review protocol. JBI Database System Rev Implement Rep. 2017 Jul;15(7):1800-1804. doi: 10.11124/JBISRIR-2016-003142. PMID: 28708743.
- Li X, Guan L, Chang H, Zhang B. Core self-evaluation and burnout among Nurses: the mediating role of coping styles. PLoS One. 2014 Dec 26;9(12):e115799. doi: 10.1371/journal.pone.0115799. PMID: 25541990; PMCID: PMC4277418.
- Rodríguez-Rey R, Palacios A, Alonso-Tapia J, Pérez E, Álvarez E, Coca A, Mencía S, Marcos A, Mayordomo-Colunga J, Fernández F, Gómez F, Cruz J, Ordóñez O, Llorente A. Burnout and posttraumatic stress in paediatric critical care personnel: Prediction from resilience and coping styles. Aust Crit Care. 2019 Jan;32(1):46-53. doi: 10.1016/j.aucc.2018.02.003. Epub 2018 Mar 28. PMID: 29605169.
- Stock E. Exploring salutogenesis as a concept of health and wellbeing in nurses who thrive professionally. Br J Nurs. 2017 Feb 23;26(4):238-241. doi: 10.12968/bjon.2017.26.4.238. PMID: 28230441.
- Antonovsky, (1979). Health, Stress and Coping. Jossey-Bass.
- Folkman S, Lazarus R. Ways of coping questionnaire manual. Mind. 1988.
- Spector PE. Measurement of human service staff satisfaction: development of the Job Satisfaction Survey. Am J Community Psychol. 1985 Dec;13(6):693-713. doi: 10.1007/BF00929796. PMID: 4083275.
- Connor KM, Davidson JR. Development of a new resilience scale: the Connor-Davidson Resilience Scale (CD-RISC). Depress Anxiety. 2003;18(2):76-82. doi: 10.1002/da.10113. PMID: 12964174.
- Kroenke K, Spitzer RL, Williams JB, Löwe B. An ultra-brief screening scale for anxiety and depression: the PHQ-4. Psychosomatics. 2009 Nov-Dec;50(6):613-21. doi: 10.1176/appi.psy.50.6.613. PMID: 19996233.
- Jakimowicz S, Perry L, Lewis J. Compassion satisfaction and fatigue: A cross-sectional survey of Australian intensive care nurses. Aust Crit Care. 2018 Nov;31(6):396-405. doi: 10.1016/j.aucc.2017.10.003. Epub 2017 Nov 16. PMID: 29153827.
- Cetrano G, Tedeschi F, Rabbi L, Gosetti G, Lora A, Lamonaca D, Manthorpe J, Amaddeo F. How are compassion fatigue, burnout, and compassion satisfaction affected by quality of working life? Findings from a survey of mental health staff in Italy. BMC Health Serv Res. 2017 Nov 21;17(1):755. doi: 10.1186/s12913-017-2726-x. PMID: 29162095; PMCID: PMC5696765.
- Goodare P. Literature review: Why do we continue to lose our nurses. Australian Journal of Advanced Nursing. 2017; 34:50-56.
- Preston A. Registered Nurses: Who are they and what do they want? Australian Bulletin of Labour. 2005; 31:321-349.
- Glied SA, Ma S, Pearlstein I. Understanding Pay Differentials Among Health Professionals, Nonprofessionals, And Their Counterparts In Other Sectors. Health Aff (Millwood). 2015 Jun;34(6):929-35. doi: 10.1377/hlthaff.2014.1367. PMID: 26056197.
- Phougeishangbam P, Mayanglambam P. Impact of COVID 19 on Health Care Personnel, Indian Journal of Public Health Research & Development. 2020; 11:79-83.https://doi-org.ezproxy.utas.edu.au/10.37506/ijphrd.v11i9.10990
- Alharbi J, Jackson D, Usher K. The potential for COVID-19 to contribute to compassion fatigue in critical care nurses. J Clin Nurs. 2020 Aug;29(15-16):2762-2764. doi: 10.1111/jocn.15314. Epub 2020 May 18. PMID: 32344460; PMCID: PMC7267232.
- Ledoux K, Forchuk C, Higgins C, Rudnick A. The effect of organizational and personal variables on the ability to practice compassionately. Appl Nurs Res. 2018 Jun;41:15-20. doi: 10.1016/j.apnr.2018.03.001. Epub 2018 Mar 3. PMID: 29853208.
- Jones J, Strube P, Mitchell M, Henderson A. Conflicts and con-fusions confounding compassion in acute care: Creating dialogical moral space. Nurs Ethics. 2019 Feb;26(1):116-123. doi: 10.1177/0969733017693470. Epub 2017 Mar 3. PMID: 29281923.
- Tusaie K, Dyer J. Resilience: a historical review of the construct. Holist Nurs Pract. 2004 Jan-Feb;18(1):3-8; quiz 9-10. doi: 10.1097/00004650-200401000-00002. PMID: 14765686.
- Galuska LA, Bursch B. Meaning, Joy, and Critical Care Nurse Well-Being: A Call to Action. Crit Care Nurs Clin North Am. 2020 Sep;32(3):349-367. doi: 10.1016/j.cnc.2020.04.002. Epub 2020 Jul 9. PMID: 32773178.
- Chang EM, Bidewell JW, Huntington AD, Daly J, Johnson A, Wilson H, Lambert VA, Lambert CE. A survey of role stress, coping and health in Australian and New Zealand hospital nurses. Int J Nurs Stud. 2007 Nov;44(8):1354-62. doi: 10.1016/j.ijnurstu.2006.06.003. Epub 2006 Aug 9. PMID: 16901488.
- McLarnon M, Rothstein M. Development and initial validation of the workplace resilience inventory. Journal of Personnel Psychology. 2013; 12:63-73.https://doi.org/10.1027/1866-5888/a000084
- Lazarus R, Folkman S. Stress, appraisal, and coping. Springer. 1984.
- Delgado C, Upton D, Ranse K, Furness T, Foster K. Nurses' resilience and the emotional labour of nursing work: An integrative review of empirical literature. Int J Nurs Stud. 2017 May;70:71-88. doi: 10.1016/j.ijnurstu.2017.02.008. Epub 2017 Feb 12. PMID: 28235694.
- Holland PJ, Tham TL, Gill FJ. What nurses and midwives want: Findings from the national survey on workplace climate and well-being. Int J Nurs Pract. 2018 Jun;24(3):e12630. doi: 10.1111/ijn.12630. Epub 2018 Feb 26. PMID: 29479760.
- Harvie K, Sidebotham M, Fenwick J. Australian midwives' intentions to leave the profession and the reasons why. Women Birth. 2019 Dec;32(6):e584-e593. doi: 10.1016/j.wombi.2019.01.001. Epub 2019 Jan 8. PMID: 30635229.
- Büssing A, Falkenberg Z, Schoppe C, Recchia DR, Poier D. Work stress associated cool down reactions among nurses and hospital physicians and their relation to burnout symptoms. BMC Health Serv Res. 2017 Aug 10;17(1):551. doi: 10.1186/s12913-017-2445-3. PMID: 28797258; PMCID: PMC5553651.
- Marin M, Garcia-Ramirez M. Social support sources and emotional exhaustion among hospital nursing staff. The European Journal of Psychiatry. 2005; 19:96-106,http://scielo.isciii.es/scielo.php?script = sci_arttext&pid = S0213-61632005000200004&lng = es&tlng = en.
- Hegney DG, Rees CS, Eley R, Osseiran-Moisson R, Francis K. The contribution of individual psychological resilience in determining the professional quality of life of Australian nurses. Front Psychol. 2015 Oct 21;6:1613. doi: 10.3389/fpsyg.2015.01613. PMID: 26539150; PMCID: PMC4612648.
- Pugh JD, Twigg DE, Martin TL, Rai T. Western Australia facing critical losses in its midwifery workforce: a survey of midwives' intentions. Midwifery. 2013 May;29(5):497-505. doi: 10.1016/j.midw.2012.04.006. Epub 2012 Nov 22. PMID: 23182501.
- McAllister M, Lee Brien D, Dean S. The problem with the superhero narrative during COVID-19. Contemp Nurse. 2020 Apr-Jun;56(3):199-203. doi: 10.1080/10376178.2020.1827964. PMID: 32969777.
- Beaumont E, Durkin M, Hollins Martin CJ, Carson J. Compassion for others, self-compassion, quality of life and mental well-being measures and their association with compassion fatigue and burnout in student midwives: A quantitative survey. Midwifery. 2016 Mar;34:239-244. doi: 10.1016/j.midw.2015.11.002. Epub 2015 Nov 6. PMID: 26628352.
- Henderson A, Jones J. Developing and maintaining compassionate care in nursing. Nurs Stand. 2017 Sep 20;32(4):60-69. doi: 10.7748/ns.2017.e10895. PMID: 29094531.
- Beaumont E, Martin C. A narrative review exploring the effectiveness of Compassion-Focused Therapy. Counselling Psychology Review. 2015; 30:21-30.
- van den Oetelaar WF, van Stel HF, van Rhenen W, Stellato RK, Grolman W. Balancing nurses' workload in hospital wards: study protocol of developing a method to manage workload. BMJ Open. 2016 Nov 10;6(11):e012148. doi: 10.1136/bmjopen-2016-012148. PMID: 28186931; PMCID: PMC5129129.
- Yilmaz. Resilience as a strategy for struggling against challenges related to the nursing profession, Chinese Nursing Research. 2017; 4:9-13. doi:http://doi.org/10.1016/j.cnre.2017.03.004
- Christodoulou-Fella M, Middleton N, Papathanassoglou EDE, Karanikola MNK. Exploration of the Association between Nurses' Moral Distress and Secondary Traumatic Stress Syndrome: Implications for Patient Safety in Mental Health Services. Biomed Res Int. 2017;2017:1908712. doi: 10.1155/2017/1908712. Epub 2017 Oct 25. PMID: 29209622; PMCID: PMC5676344.
- Mills J, Chamberlain-Salaun J, Harrison H, Yates K, O'Shea A. Retaining early career registered nurses: a case study. BMC Nurs. 2016 Oct 10;15:57. doi: 10.1186/s12912-016-0177-z. PMID: 27766042; PMCID: PMC5057224.
- Hegney DG, Rees CS, Osseiran-Moisson R, Breen L, Eley R, Windsor C, Harvey C. Perceptions of nursing workloads and contributing factors, and their impact on implicit care rationing: A Queensland, Australia study. J Nurs Manag. 2019 Mar;27(2):371-380. doi: 10.1111/jonm.12693. Epub 2018 Sep 17. PMID: 30221436.
- Stamm B. Measuring compassion satisfaction as well as fatigue: Developmental history of the compassion satisfaction and fatigue test. In C.R. Figley (Ed.). Treating compassion fatigue. 2002; 107-119. Brunner-Routledge.
- Wang J, Okoli CTC, He H, Feng F, Li J, Zhuang L, Lin M. Factors associated with compassion satisfaction, burnout, and secondary traumatic stress among Chinese nurses in tertiary hospitals: A cross-sectional study. Int J Nurs Stud. 2020 Feb;102:103472. doi: 10.1016/j.ijnurstu.2019.103472. Epub 2019 Nov 13. PMID: 31810017.

Article Alerts
Subscribe to our articles alerts and stay tuned.
 This work is licensed under a Creative Commons Attribution 4.0 International License.
This work is licensed under a Creative Commons Attribution 4.0 International License.

 Save to Mendeley
Save to Mendeley
